Alarm Over Falling Vaccination Rates in Ontario Sparks Measles Concerns
2024-12-22
Author: Benjamin
Alarm Over Falling Vaccination Rates in Ontario Sparks Measles Concerns
In a troubling trend, recent data from Public Health Ontario reveals that only 70% of seven-year-olds in the province were fully vaccinated against measles in the past year. This decline is a stark contrast to the pre-pandemic era, when the vaccination coverage stood at an impressive 94% during the 2013-2014 school year.
The concerning figures raise alarms about herd immunity, which is essential for preventing outbreaks of this highly contagious disease. Experts note that herd immunity for measles requires at least 90%-95% of a population to be vaccinated. With the current vaccination rate hovering at just 70%, Ontario is at a significant risk.
Vaccination coverage varies widely across different regions. In Peel Region, part of the Greater Toronto Area, fewer than 25% of seven-year-olds were fully vaccinated against measles. Similarly, Ottawa also showed disappointing numbers, with only 64% of children in this age bracket vaccinated—down from 94.5% in 2016-2017.
Interestingly, while younger children face lower vaccination rates, 17-year-olds in the province maintain a much healthier vaccination level, boasting an average of around 91% coverage for measles. This discrepancy raises questions about access and compliance among younger populations.
The decline in immunization rates has been attributed to a combination of factors. Public health officials recognize that disruptions caused by the COVID-19 pandemic and the current shortage of family doctors have played significant roles. This situation is exacerbated by the province's complex and often disjointed immunization records system, which hampers the accurate tracking of vaccination status. Many vaccinations administered by family physicians do not get reported automatically to public health units, leaving gaps in the data.
Marie-Claude Turcotte, Director of Community Wellness and Chronic Disease Prevention at Ottawa Public Health, highlighted that over 15,000 students in Ottawa, specifically born in 2007 and 2017, are missing one or more vaccines from their public health records. These numbers raise the urgency for interventions, as public health initiatives aim to close these gaps.
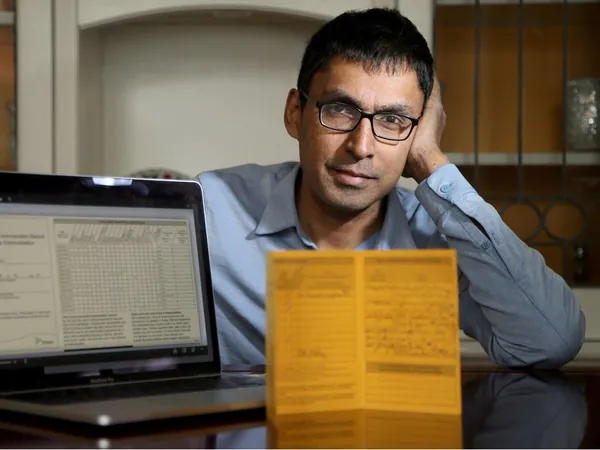
Dr. Kumanan Wilson from The Ottawa Hospital voiced concerns that the current data might not fully reflect the reality on the ground, emphasizing that while measles is indeed circulating globally, Ontario has not yet seen a corresponding outbreak. This suggests that the reported vaccination rates may not be entirely accurate, particularly when national surveys indicate a measles vaccination coverage of approximately 88%.
Further complicating the issue is the resurgence of whooping cough across Canada, with areas such as eastern Ontario and Ottawa hit particularly hard. Last year, just 62% of seven-year-olds in Ottawa were vaccinated against pertussis, below the provincial average of 69.8%.
In response to these pressing challenges, Ottawa Public Health is implementing strategies such as targeted outreach to families with unvaccinated children and possible repercussions for non-compliance, such as suspension from school. Additionally, there are calls from the Ontario Immunization Advisory Committee for a more robust vaccine registry system, emphasizing the need for immediate improvements in the documentation and tracking of vaccinations.
As vaccine hesitancy grows—fueled by misinformation and the political landscape—it's essential for provinces like Ontario to address these challenges head-on. With fewer people getting vaccinated, the risk of widespread outbreaks for vaccine-preventable diseases increases significantly, threatening public health and putting vulnerable populations at greater risk.
This situation underscores the need for improved educational initiatives and a reevaluation of how vaccinations are tracked and reported. Public health measures are more crucial than ever to ensure that children receive the vaccinations they need to protect their health and the health of their communities.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)