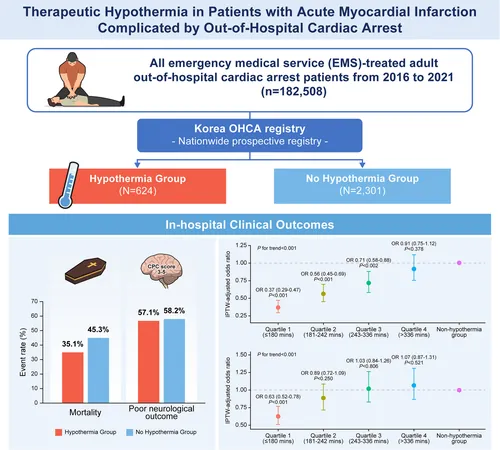
Groundbreaking Study Reveals Therapeutic Hypothermia Saves Lives in Cardiac Arrest Survivors
2025-03-26
Author: Jacob
Overview
Recent research has illuminated the complexities of managing patients who suffer from acute myocardial infarction (AMI) coupled with out-of-hospital cardiac arrest (OHCA), revealing the life-saving potential of therapeutic hypothermia. As healthcare professionals navigate the challenges of post-cardiac arrest care, the findings suggest that this treatment could significantly impact patient survival rates.
What is Therapeutic Hypothermia?
Therapeutic hypothermia is a medical treatment that reduces body temperature to help protect the brain after cardiac arrest. The aim is to lower metabolic demands on the brain and increase its chances of recovery.
Study Background
Conducted using a prospective nationwide registry from 2016 to 2021, this comprehensive study analyzed data from 2,925 patients who experienced AMI and underwent urgent percutaneous coronary intervention (PCI) following OHCA. Out of these, 624 patients received therapeutic hypothermia, while 2,301 did not.
Key Findings
1. Reduced Mortality Rates: The group that underwent therapeutic hypothermia experienced significantly lower in-hospital mortality rates (35.1%) compared to the non-hypothermia group (43.3%). This translates to a 29% reduction in the odds of death (odds ratio [OR] 0.71), a finding that underscores the potential benefit of early temperature management.
2. Impact of Timing: A critical factor highlighted in the study was the "door-to-cooling" (DtC) time, the period from hospital arrival to the commencement of hypothermia treatment. Shorter DtC times were correlated with even lower mortality rates and enhanced chances of favorable neurological outcomes. Patients treated in the fastest quartile (≤180 minutes) had an astonishing OR of 0.40 for mortality compared with those treated in the slowest quartile.
3. Neurological Outcomes: Despite the impressive mortality benefits, it is essential to note that therapeutic hypothermia did not demonstrate significant improvements in neurological outcomes at discharge. This aspect of the study invites further exploration into optimizing protocols to enhance brain recovery.
Protocol Insights
The study also compared various hypothermia protocols, including temperature settings (33°C vs. 36°C) and treatment durations (24 hours vs. 48 hours). Interestingly, the results showed no significant differences in outcomes based on these variations.
Implications for Clinical Practice
These findings highlight the urgency for medical teams to consider implementing therapeutic hypothermia quickly in patients following OHCA with AMI. Furthermore, the call for more standardized protocols is crucial to maximize both survival and neurological recovery.
Future Directions
As the medical community reviews these results, ongoing and future research is necessary to define optimal duration and parameters for hypothermia therapy. The ongoing Influence of Cooling Duration on Efficacy in Cardiac Arrest Patients (ICECAP) trial seeks to answer these pivotal questions.
Conclusion
This landmark study adds to the growing body of evidence supporting the use of therapeutic hypothermia as a life-saving intervention for patients suffering from AMI complicated by OHCA. While the focus on immediate survival outcomes is critical, future research must address the nuances of neurological recovery to enhance the holistic treatment of cardiac arrest survivors.
By shining a light on the need for effective therapeutic interventions, such as hypothermia, we can continue to improve survival and quality of life for patients who endure these life-threatening events.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)