Ozempic and Wegovy: A New Era of Drug Coverage in Canada?
2025-01-14
Author: Charlotte
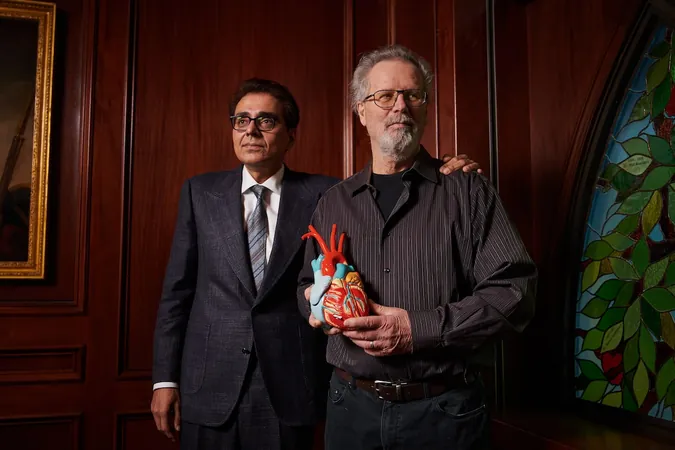
After surviving a heart attack and double bypass surgery in 2019, Richard Neilson, a 68-year-old truck driver from Toronto, entered a clinical trial for a groundbreaking medication called semaglutide, now widely known as Ozempic. Initially aimed at reducing his risk of future heart attacks, Mr. Neilson found himself benefiting in an unexpected way—he lost 45 pounds while participating in the trial for Wegovy, the higher-dose version of semaglutide designed for weight management.
In November 2022, Health Canada made a pivotal decision by approving Wegovy for cardiovascular risk reduction, marking it as the first GLP-1 receptor agonist to receive this designation outside the realm of diabetes and obesity. This significant regulatory development aligns with the growing body of evidence suggesting that GLP-1 medications could offer health benefits extending beyond weight loss.
The trend doesn't stop there. The U.S. Food and Drug Administration (FDA) recently approved a similar drug, tirzepatide, sold under the name Zepbound, for obstructive sleep apnea. The research into GLP-1 drugs is expansive, with potential applications spanning chronic kidney disease, non-alcoholic fatty liver disease, and even neurodegenerative conditions such as Alzheimer’s and Parkinson's diseases.
With the expansion of uses for these medications, Canadian public drug plans are confronting challenges in coverage, particularly against the backdrop of already strained healthcare budgets. Currently, coverage for Ozempic is restricted strictly to diabetes patients, while Wegovy has been excluded from coverage due to its weight management classification. This limitation could be reversed if compelling evidence mounts for broader chronic illness treatment.
Mina Tadrous, a pharmaceutical policy expert at the University of Toronto, anticipates a shift in how insurers approach coverage for weight-loss medications, traditionally viewed as elective or cosmetic. As more data emerge supporting the cardiovascular and overall health impacts of GLP-1 drugs, there is a growing recognition that managing such medications is no longer just about vanity but about essential health improvements.
The mechanism of GLP-1 drugs involves imitating the GLP-1 hormone, promoting blood sugar control and weight loss through slow gastric emptying and reduced appetite. While common side effects include nausea, recent analyses highlight potential anti-inflammatory benefits that might contribute to improved outcomes in heart disease and other chronic conditions.
Ozempic continues to dominate the Canadian pharmaceutical landscape, with nearly $2.3 billion in sales through retail pharmacies in 2022—more than double that of its closest competitor, Stelara. Wegovy, which debuted in Canada last year, accumulated sales nearing $147 million within just a few months of its launch.
As the financial burden of these medications rises, more Canadians are calling out for equitable access. Subodh Verma, a professor at the University of Toronto, advocates for reconsidering the inclusion of Wegovy in coverage discussions, emphasizing its necessity beyond aesthetics—pointing out that it may significantly benefit patients with cardiovascular risks.
Neilson, unfortunately, found himself unable to afford Wegovy after his trial participation ended, despite being eligible for support under Ontario’s Drug Benefit Program, which does not cover Wegovy. This scenario is increasingly common; many patients in need of GLP-1 drugs for conditions such as diabetes, obesity, or heart disease are unable to access them due to a lack of funding.
In an effort to improve accessibility, pharmaceutical company Novo Nordisk is actively engaging with various stakeholders, advocating for the recognition of obesity as a chronic disease and paving the road toward better drug coverage. As the Canadian Drug Agency reevaluates Wegovy’s status in light of its new approval, the question remains: will insurers finally adapt to meet the demand for more inclusive drug coverage?
As healthcare continues to evolve, the narrative is shifting from merely managing weight to prioritizing holistic health outcomes, a change that could redefine drug access and patient care in Canada in the near future.









 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)