
Revolutionary 999 Call Scheme Reduces Mental Health Crisis Emergency Room Visits by 40%!
2024-11-20
Author: Michael
Introduction
In an innovative pilot project within the South Eastern Health Trust area, a collaboration between mental health nurses and the Northern Ireland Ambulance Service (NIAS) has yielded remarkable results, demonstrating a stunning 40% decrease in the number of individuals in mental health distress being admitted to emergency departments (EDs).
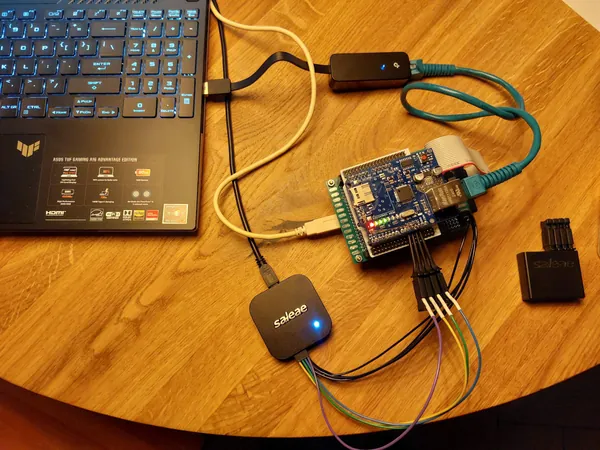
Project Overview
This groundbreaking initiative, funded by the Public Health Agency (PHA), features a dedicated team of 12 mental health practitioners stationed in the NIAS control room in Belfast, providing support during high-demand periods, specifically on weekends.
Purpose of the Scheme
Designed to cater to individuals who seek help during a mental health crisis, the scheme enables mental health professionals to conduct assessments over the phone, ensuring that those in distress receive the appropriate care without the need for an ambulance or an ED visit—often an inappropriate setting for individuals grappling with issues like depression and anxiety.
Impact and Statistics
Project lead Stephanie Patten shared insights regarding the significant impact of this program, stating, "Between April and September, we received 190 calls related to mental health crises, and 40% of those were able to be de-escalated." This means that many individuals were able to receive immediate support without the frustrations of waiting for an ambulance or sitting in a crowded emergency room.
Practitioner Responses
The response from the mental health practitioners is empathetic and thorough. Anne-Marie Scott, one of the nurses engaged in this scheme, elaborated on the process: "We listen intently to the callers, allowing them to express their feelings. Our goal is to help them rationalize their emotions and, if needed, guide them towards statutory or voluntary services for further assistance."
Operational Timing
The scheme operates during critical times, specifically on Friday and Saturday nights and Sunday afternoons into the evening. When a 999 call is made for a mental health crisis, operators are trained to transfer these calls to mental health nurse practitioners who provide immediate evaluation and support.
Service Gap Addressed
This initiative addresses a significant gap in mental health care during off-hours when traditional services may not be readily available. Karl Bloomer, a consultant paramedic with NIAS, noted the surge in mental health calls during these hours, stating, “Oftentimes, 999 and ED services aren’t the most suitable options for these patients, and we are thrilled to properly target emergency ambulance responses.”
Support for NIAS Staff
Additionally, an often-overlooked advantage of the project is how it supports NIAS staff themselves during challenging calls. The mental health practitioners offer guidance and expertise, bolstering the confidence and capability of those in the control room.
Integration of Digital Health Records
With the integration of the Encompass digital health records system, this program is now able to extend its reach, potentially improving the care provided to patients from the Belfast Trust area as well.
Looking Ahead
Looking ahead, stakeholders are optimistic about the expansion of this life-saving initiative. Mr. Bloomer expressed an ideal vision, “We hope to see this service operational seven days a week across the region.”
Conclusion
This pioneering project not only showcases the importance of targeted mental health support but also sets a precedent that could reshape emergency response protocols across the nation. The positive results are clear: timely and compassionate care during a crisis can make all the difference!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)