Revolutionizing Cervical Cancer Screening: New Home Testing Protocol Promises Fewer Clinician Follow-Ups for Women
2024-12-13
Author: Benjamin
Introduction
A groundbreaking new protocol for analyzing self-collected cervical samples is poised to significantly reduce the number of women who need follow-up clinician screenings. This innovative approach not only streamlines the cervical cancer screening process within the NHS but also facilitates faster referrals for gynecological assessments when necessary.
Study Overview
Led by researchers from Queen Mary University of London, the study examined data related to each self-sample to gauge the risk of significant disease presence. This method aims to minimize unnecessary recalls for clinician-collected samples while allowing high-risk patients to be directed straight to secondary care, which could dramatically enhance the overall effectiveness of cervical cancer detection.
Publication and Context
Published in the esteemed journal PLOS Medicine, this research sheds light on the pressing issue of cervical cancer, one of the most preventable cancers. Despite its preventability, statistics reveal that participation in the NHS Cervical Screening Program has reached historic lows. To combat this, self-sampling HPV tests—which empower women to collect their own samples at home—are being explored as a strategy to boost screening rates.
Public Preference
Notably, Queen Mary’s recent findings indicate that nearly 70% of women prefer self-sampling if given the option. The UK National Screening Committee is currently considering the implementation of HPV self-sampling for individuals who have not previously been screened via the NHS program, marking a significant potential shift in public health resources.
Limitations of Home-collected Samples
In contrast to traditional clinician-collected samples, which necessitate a visit to a General Practitioner, home-collected samples pose limitations as they cannot be processed through cytology. A follow-up clinician sample is essential when HPV is detected, further complicating the process and leading to a potentially alarming situation where one in five women fail to follow through with necessary testing after a positive self-sample.
Research Findings
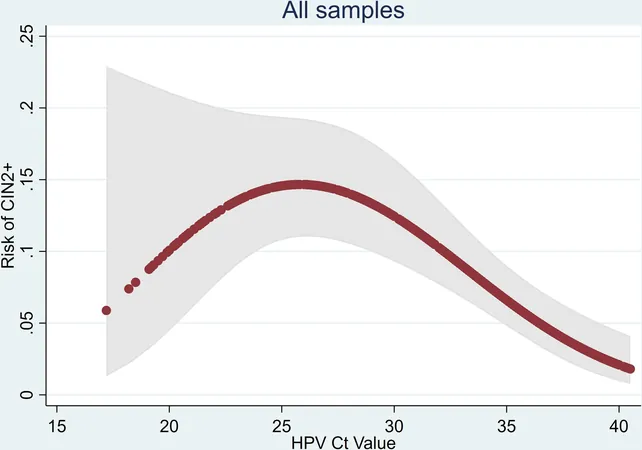
The research team, led by Professor Peter Sasieni, utilized enhanced HPV test results that are typically excluded from analysis. They categorized HPV-positive women into three risk groups: high-risk, medium-risk, and low-risk. Alarmingly, only 5% of participants were classified as high-risk, yet nearly 40% of this group exhibited diseases that warranted immediate treatment.
Conclusion
Encouragingly, about 53% fell into the low-risk category, with only a mere 4% confirming high-grade disease. This posits that these women could safely undergo re-testing after a year without the need for immediate clinician intervention, potentially preventing unnecessary anxiety and health complications.
Expert Opinion
Professor Sasieni, a renowned expert in cancer epidemiology and co-lead of the Center for Cancer Screening, Prevention, and Early Diagnosis at the Wolfson Institute of Population Health, advocates for the new risk assessment protocol. He stated, "Our analysis suggests it is safe for most women with a positive self-sample to wait for re-testing after 12 months instead of undergoing further clinician sampling. This will not only reduce the number of unnecessary clinician visits but also ensure early detection of cancer in most cases."
Impact on Women's Health
In a time when cervical cancer screening is critical, this new protocol offers a beacon of hope—transforming the paradigm of how women engage with their health and reducing the barriers that have previously hindered effective screening. As we await wider implementation, this groundbreaking method could redefine cervical health and save lives in the process.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)