Revolutionizing Type 1 Diabetes Treatment: Can Stem Cells Provide a Cure?
2024-11-20
Author: Liam
Type 1 diabetes (T1D) is a relentless adversary that wreaks havoc on the body’s ability to regulate blood glucose levels. Classified as an autoimmune disorder, T1D arises when the immune system erroneously identifies insulin-producing beta cells in the pancreas as intruders, leading to their destruction. This process can shatter the lives of affected individuals, stealing an average of 32 years of healthy living.
Currently, the standard treatment for T1D hinges on lifelong insulin injections. While these injections can manage glucose levels, they come with the constant threat of hypoglycemia—a dangerous condition marked by abnormally low blood sugar levels. Symptoms of hypoglycemia can range from mild (shakiness, irritability) to severe (confusion, seizures), posing significant health risks. Although continuous glucose monitors and automated insulin delivery systems provide some relief, they’re not a catch-all solution for every patient.
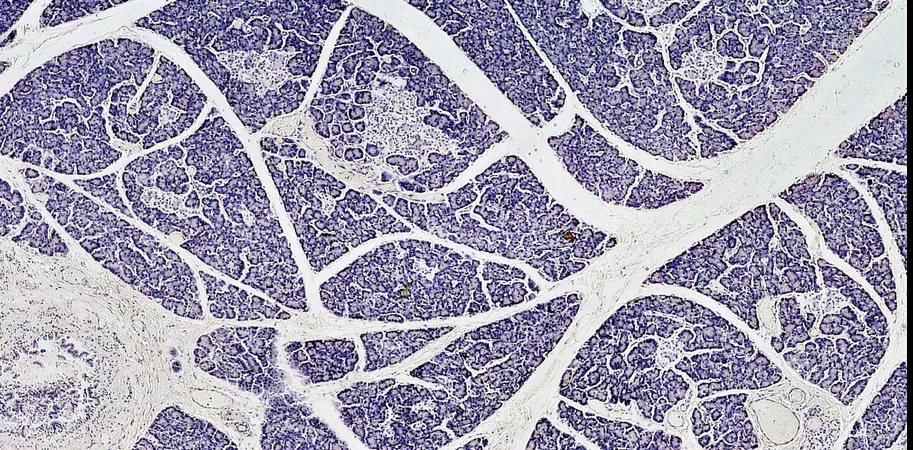
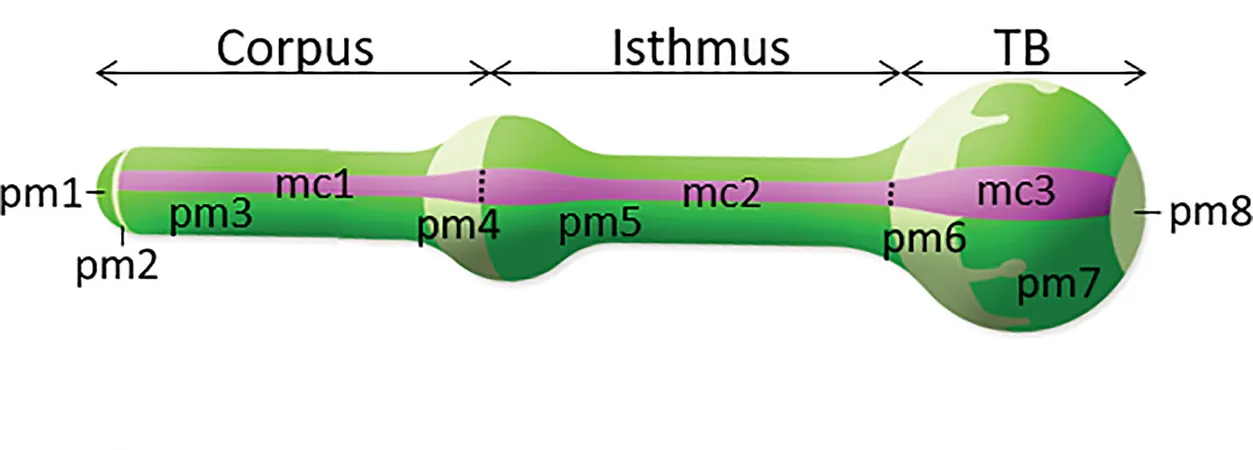
An exciting alternative is islet transplantation, a procedure that involves transplanting clusters of insulin-producing cells from a donor's pancreas. This approach has the potential to restore the body’s natural ability to regulate glucose. However, the procedure is limited by the scarcity of donor organs and the necessity of lifelong immunosuppressant medications. As a result, only about 10% of individuals with T1D qualify for this treatment.
In my quest as a diabetes researcher, my team and I have been exploring the groundbreaking possibilities that stem cells can offer to surmount these hurdles.
A Journey Through Islet Transplantation History
Islet transplantation for T1D finally received FDA approval in 2023, capping over a century of persistent research and experimentation. The islets of Langerhans, the pancreatic clusters that house beta cells, were first identified in 1869 by scientist Paul Langerhans. Despite setbacks—from the early experimental sheep pancreatic transplants that ended in tragedy to several unsuccessful human trials—progress was made in the latter half of the 20th century. The breakthrough came in 1999 when James Shapiro's team in Edmonton successfully demonstrated a protocol that allowed patients to manage their diabetes without insulin for a year, leading to the wider acceptance of islet transplantation as a viable treatment.
Unlocking the Potential of Stem Cells
While islet transplantation is now a relatively minor procedure, it faces significant challenges, including steep costs, limited availability of donor islets, and the risks associated with long-term immunosuppressive therapy. To tackle these issues, researchers are shifting their focus to stem cells, which could provide a virtually limitless supply of islets.
Two primary types of stem cells are currently under investigation: embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). While both can differentiate into insulin-producing islets in the lab, they possess distinct benefits and drawbacks. ESCs, which are derived from human embryos, face ethical issues and still require immunosuppressants for transplant. In contrast, iPSCs can be generated from a patient's own skin, blood, or fat cells, potentially eliminating the need for immunosuppressive drugs. However, the costs of developing patient-specific iPSCs remain a substantial barrier.
The Challenges Ahead
Despite their promise, iPSCs are not a panacea. For T1D patients with specific genetic mutations, the very cells harvested to generate iPSCs may carry the same detrimental traits as their diseased beta cells. Fortunately, advancements in gene editing show potential for correcting these mutations before transplantation.
Moreover, the financial burden of stem cell-derived islet transplantation—likely more expensive than traditional insulin therapy—poses an additional challenge. Researchers are exploring solutions such as biobanks for iPSC compatibility, which would facilitate the use of existing stem cells for multiple patients, thus driving down costs.
There's also the potential risk of tumors developing from stem cell-derived islets. While current studies in both animal models and initial human trials have reported minimal instances of cancer, this risk remains a critical consideration moving forward.
As the field strives for breakthroughs, there is hope that with continued research and innovation, stem cell-derived islets could transform the landscape of Type 1 diabetes treatment. The path is intricate and laden with challenges, but the relentless pursuit to not just manage but possibly cure diabetes may soon lead to a future where this disease no longer rules lives. Stay tuned as we unravel the mysteries of the medical frontier!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)