Safety and Efficacy of Adjuvant CDK4/6 Inhibitors in HR+ Breast Cancer: A Closer Look at Ribociclib and Abemaciclib
2024-12-22
Author: Jacques
Case Summary
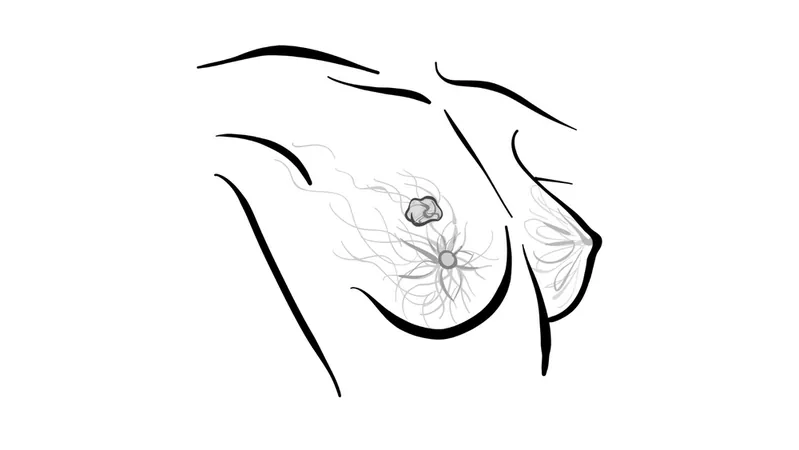
In a recent clinical evaluation, a 52-year-old woman underwent routine mammogram screening that revealed a 1.9-cm mass in her left breast. Subsequent examinations, including ultrasound, confirmed the mass's presence. A core biopsy revealed a grade 3 invasive ductal carcinoma (IDC) with hormonal receptor positivity — estrogen receptor 80%, progesterone receptor 25%, and HER2 negativity. The 21-gene recurrence score was determined to be 25, with a Ki-67 proliferation index of 25%. After confirming the absence of metastatic disease through PET-CT and a sentinel lymph node biopsy, she underwent a left mastectomy, where the tumor size was confirmed at 2.1 cm and staged at T2pN0M0/IIA.
Safety Profile of Ribociclib in the NATALEE Trial
The NATALEE trial (NCT03701334) investigated the safety profile of ribociclib (Kisqali) in patients with high-risk HR+ breast cancer. Notably, neutropenia emerged as the primary toxicity observed, affecting 62% of participants, with 42% experiencing grade 3 neutropenia. Other reported toxicities included arthralgia and nausea, but liver function tests showed a concerning trend, with 19% of patients displaying elevated alanine aminotransferase (ALT) levels (6% grade 3) and 16% with elevated aspartate aminotransferase (AST) levels (4% grade 3).
Adverse event-related discontinuations occurred in 19% of the trial population, with a median time to discontinuation at 4 months due to toxicities. The consistent monitoring of blood values enabled early identification of these adverse effects, allowing for timely dose adjustments or treatment interruptions.
Pharmacokinetics and Efficacy of Dose Reduction
Interestingly, maintaining efficacy remains feasible even with dose reductions in ribociclib treatment. Recent analysis presented at the European Society for Medical Oncology Annual Congress indicated that lowering the dose from 400 mg to 200 mg did not compromise the treatment's efficacy, aligning with findings from prior studies like the monarchE trial.
The updated data also revealed discontinuation rates steady at 20%, with liver-related adverse events cited as the most common reason for discontinuation. Meanwhile, grade 3 QT prolongation was minimal, and interstitial lung disease occurrences were very low, emphasizing the safety of ribociclib when used cautiously.
Choosing Between Ribociclib and Abemaciclib
The choice between ribociclib and abemaciclib hinges on patient-specific factors, including safety profiles and pre-existing comorbidities. Ribociclib's treatment duration spans three years compared to abemaciclib's two years, which might influence treatment strategies for high-risk patients. Notably, ribociclib's dose is set lower (400 mg) in the early stages compared to higher doses used in metastatic settings, adding a layer of complexity to treatment planning.
Patients experiencing intolerable side effects from one drug may benefit from a switch to the other, offering a tailored approach to managing the adverse effects of CDK4/6 inhibitors.
Common Treatment Challenges and Considerations
For abemaciclib, diarrhea remains the most common adverse effect, occurring in 84% of patients and resulting in a 19% discontinuation rate, particularly in the initial treatment months. As doctors manage treatment for older patients, careful monitoring and educating them about potential side effects could help improve adherence to therapy.
Practical considerations include differing tablet strengths and dosing schedules between the two drugs. Ribociclib is administered at 400 mg via two 200 mg tablets, while abemaciclib starts at 150 mg taken twice daily. As the FDA explores optimizing CDK4/6 inhibitor dosing strategies, the emphasis on personalized treatment based on individual pharmacokinetics continues to gain traction.
Conclusion
In summary, the comparison of ribociclib and abemaciclib underlines the need for careful consideration of safety, efficacy, and patient tolerance in managing HR+ breast cancer. As more research emerges, oncologists are better equipped to refine their treatment strategies for optimal patient outcomes. Stay tuned for more updates in the ongoing battle against breast cancer!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)