Shocking Consequences: How COVID-19 Lockdowns Devastated Tuberculosis Treatment Adherence in South Africa
2024-10-14
Author: Sophie
Introduction
The COVID-19 pandemic has wreaked havoc on health systems globally, but its impact on tuberculosis (TB) treatment, particularly through directly observed therapy (DOT) programs, remains alarming. A recent study compared TB treatment adherence during the pandemic in South Africa, revealing unsettling data that could have lasting implications for public health.
Context of the Study
As South Africa faced its first COVID-19 case on March 5, 2020, a national lockdown was swiftly imposed. This lockdown enforced severe restrictions, resulting in millions being confined to their homes, with schools and businesses shuttered. The ramifications on healthcare systems, especially for TB—a disease that the country has long battled—were immediate and profound.
Research Design and Methodology
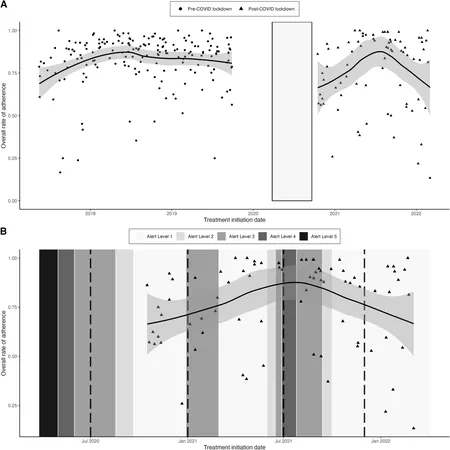
In a thorough investigation, researchers analyzed data from 263 TB patients who participated in a DOT program from May 2017 to March 2022. Participants were categorized into two groups: those treated before the pandemic and those treated after the lockdowns ended. Advanced statistical techniques were employed to isolate the effects of COVID-19 on DOT adherence, controlling for various factors such as demographic profiles, mental health conditions, and socioeconomic status.
Key Findings: An Alarming Rise in Non-Adherence
The study revealed a staggering 42% higher rate of non-adherence to DOT in patients enrolled post-lockdown compared to their pre-COVID counterparts. Immediately after the lockdowns, this rate peaked at an alarming 74%. The investigation identified several critical barriers exacerbated by the pandemic. Patients enrolling during this tumultuous time showed significantly higher levels of unemployment, severe undernourishment, and depression. In fact, 73.8% of individuals in the post-lockdown cohort were unemployed, compared to 59% pre-COVID.
The Broader Implications for TB Treatment
It's important to acknowledge that medication non-adherence is a leading cause of unfavorable TB outcomes, and many factors contribute to this issue. The pandemic introduced new stresses, leading to disruptions in DOT programs, including reduced contact between healthcare workers and patients. A shocking statistic from elsewhere showed that in certain regions of India, only 2% of TB patients in DOT programs maintained supervision during the lockdown.
Adaptations and Adjustments During the Pandemic
In response to these challenges, the study’s DOT protocols were modified to prioritize safety. Community health workers adjusted their approaches, implementing strict hygiene measures and conducting home visits outdoors to ensure continuing medication adherence. However, even with these adaptations, the overall treatment adherence did not bounce back to pre-pandemic levels, sparking concerns about the effectiveness of TB management strategies in times of global health crises.
Conclusion: A Call to Action
As we reflect on these findings, it becomes clear that the COVID-19 pandemic's impact extends beyond immediate health concerns; it has created long-term barriers to TB treatment adherence in South Africa. The findings emphasize the urgent need for targeted interventions aimed at overcoming the exacerbated barriers to adherence, particularly among high-risk populations.
Looking Forward
The study underscores an immediate and significant need for health authorities to strategize recovery efforts that prioritize mental health and food security, ensuring that populations vulnerable to TB receive uninterrupted treatment support. Understanding the persistent effect of the pandemic on TB programs can guide future public health policies to build a resilient framework capable of withstanding such crises.
In sum, the consequences of COVID-19 on TB treatment adherence reveal a troubling landscape that must be urgently addressed to safeguard the health of millions. We can no longer afford to ignore the shadows cast by this global pandemic on long-term health outcomes.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)