Unlocking the Secrets of Ovarian Cancer: How Radiomics and Radiogenomics Are Revolutionizing Diagnosis and Prognosis
2024-12-14
Author: Olivia
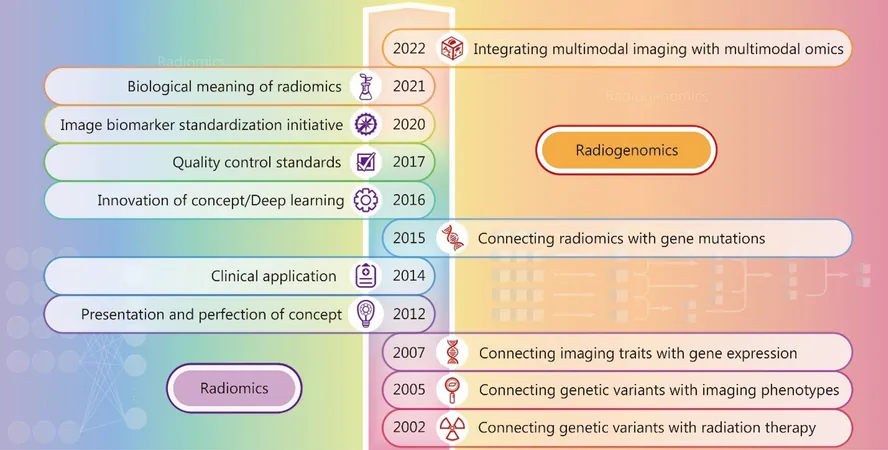
In the rapidly evolving field of oncology, radiomics and radiogenomics are pioneering new methodologies to extract critical information from medical images, significantly enhancing the diagnosis and prognosis of ovarian cancer (OC). This innovative approach harnesses the power of advanced imaging analytics to offer objective and quantitative evaluations of tumor characteristics, facilitating better patient outcomes.
The Promising Future of Radiomics in Ovarian Cancer Diagnosis
The accurate classification of ovarian masses is crucial to develop effective treatment strategies. Traditional imaging techniques often struggle to differentiate benign from malignant tumors due to overlapping morphological features. This predicament frequently leads to misdiagnoses, resulting in poor patient prognoses. To address this, researchers have turned to radiomics, which analyzes advanced imaging data to classify and subtype ovarian tumors.
For instance, groundbreaking studies have utilized machine learning algorithms to analyze ultrasound and MRI images, yielding impressive metrics such as an area under the receiver operating characteristic (ROC) curve (AUC) of 0.997 in distinguishing between benign and malignant tumors. Further advancements in studies like those by Li et al. have demonstrated competing models using contrast-enhanced CT images, achieving AUCs as high as 0.96. These findings showcase the significant potential of artificial intelligence and imaging to enhance diagnostic precision.
Navigating the Complexity of Borderline Ovarian Tumors
With the recognition that borderline ovarian tumors (BOTs) differ from benign and malignant tumors, researchers are now focusing on distinguishing these lesions more effectively. Recent studies leveraging 3D MRI radiomics have showcased the ability to achieve a perfect AUC of 1.000 in accurately identifying BOTs. Such advancements not only refine the diagnostic process but also enable more personalized treatment approaches, thereby improving patient outcomes.
Subtyping for Tailored Treatments
Not all ovarian cancers are created equal. Understanding the distinction between different subtypes—such as high-grade serous ovarian carcinoma (HGSOC) and low-grade serous ovarian carcinoma (LGSOC)—is essential for determining the appropriate management strategies. Radiomics analysis has emerged as a viable alternative to conventional biopsy methods, allowing non-invasive tumor assessments that can guide therapy options based on clinical behavior and biology.
Research indicates that HGSOC typically integrates better responses to neoadjuvant chemotherapy compared to non-HGSOC subtypes. As such, distinguishing between these subtypes before treatment is imperative and could lead to improved survival rates. Radiomics models are rapidly developing to fill this crucial gap, offering promising AUC metrics that demonstrate their efficacy in clinical practice.
Prognostic Prediction: A Game Changer for Patient Care
The ability to predict outcomes for ovarian cancer patients based on preoperative imaging enhances clinicians’ capabilities to tailor individual treatment plans. Radiomics has been shown to identify patients at high risk for poor outcomes even before surgery, providing critical insights for potentially more aggressive therapeutic interventions.
Recent predictive models have effectively used imaging characteristics to assess survival, with studies reporting promising results—such as an AUC of 0.822 when predicting overall survival using deep learning models. However, broader validation of these models across different healthcare settings is necessary to ensure they can be reliably implemented in practice.
Towards a Future of Integrated Treatment Decisions
Radiogenomics adds another layer to this evolving landscape, combining imaging data with genetic insights. By evaluating gene mutations associated with ovarian cancer and correlating them with radiomic features, healthcare providers can gain an integrated view of tumor behavior, guiding treatment decisions and improving prognostic outcomes further.
Particularly, the identification of BRCA mutations and cyclin E1 amplifications through radiogenomic approaches could streamline treatment strategies, leveraging personalized therapies that align with patients’ genetic profiles. As researchers continue to explore the relationship between imaging characteristics and genetic changes, we anticipate even greater strides in successful OC management.
Conclusion: The Path Ahead
The integration of radiomics and radiogenomics heralds a transformative era in the diagnosis and treatment of ovarian cancer. With continued advancements in technology and analytical techniques, there lies a significant opportunity for precision medicine to reshape clinical paradigms catering to individual patient needs. The potential for early diagnosis, personalized therapy, and improved prognostic stratification paints an optimistic future in the fight against this challenging disease.
As research progresses, it will be critical to ensure that these exciting technologies are validated and made accessible to the global healthcare community, enhancing treatment outcomes for ovarian cancer patients worldwide.
Stay tuned as we uncover more groundbreaking developments in the dynamic intersection of radiomics, radiogenomics, and oncology!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)