
Unraveling the Myeloid Landscape in Rheumatoid Arthritis: A Breakthrough in Treatment Strategies!
2024-12-16
Author: Sophie
Rheumatoid arthritis (RA) is a debilitating autoimmune condition known for inflicting relentless joint inflammation that can lead to severe pain and long-term disability. Despite advances in medical treatments, a significant number of patients do not experience adequate relief, making it imperative to pinpoint predictors of disease progression and therapeutic responses. A recent study aims to shed light on the pivotal role of macrophages in RA pathogenesis, offering a glimmer of hope in the quest for more effective treatments.
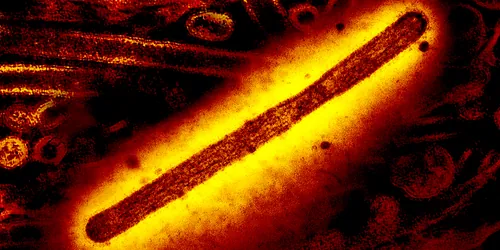
Macrophages: The Unsung Heroes and Villains of RA
Macrophages are critical immune cells that orchestrate inflammation and tissue remodeling. This groundbreaking study examined the populations of macrophages residing within the synovium of RA patients, individuals at risk of developing RA (IAR), and healthy controls. What researchers found was transformative.
A Distinct Macrophage Subset Linked to RA Progression
The study unveiled a unique macrophage subset enriched in the inflamed joints of RA patients. Characterized by the high expression of CD206 and CD163—markers associated with healing—these macrophages also expressed elevated levels of CD40, typically linked to pro-inflammatory M1 macrophages. This peculiar combination suggests that instead of merely repairing tissue, this population actively contributes to disease progression, casting a new light on their role in RA pathology.
Chronic Inflammation: The Macrophage Invasion
Through flow cytometric analysis, researchers noted a striking increase in the prevalence and intensity of macrophage markers (CD68 and CD64) in the synovial tissue, indicating that these immune cells accumulate significantly during active disease. The findings reveal a surprising complexity in macrophage behavior; rather than falling neatly into M1 or M2 categories, these cells exhibit a variety of activation states, underscoring their adaptive responses to the RA joint's fluctuating microenvironment.
Profiling Macrophage Populations: The Genetic Blueprint
Employing advanced RNA sequencing techniques, scientists discovered a unique transcriptional profile within the CD206+CD163+ macrophage population, distinct from other macrophage types. This signature related to inflammatory processes and tissue residency hints at their vital role in disease activity and joint remodeling, positioning them as critical players in the RA landscape.
Single-Cell Analysis Reveals Macrophage Diversity
Single-cell RNA sequencing (scRNA-seq) further illuminated the diversity within macrophage populations, identifying an astonishing nine distinct macrophage clusters among 67,908 cells analyzed. Among these clusters, two subsets marked with IL-1B+CCL20+ and SPP1+MT2A+ demonstrated a heightened expression of CD40, further reinforcing their influential role in chronic inflammation. Notably, these specific macrophage populations were already present before the clinical onset of RA, indicating they may play a crucial role in early disease development.
Transforming Diagnosis and Treatment Approaches
These revelations carry significant implications for the early diagnosis and treatment of RA. The identification of the CD40-expressing CD206+CD163+ macrophage subset as an early biomarker may allow clinicians to detect the disease in its nascent stages, opening avenues for preemptive strategies that could delay or even halt disease progression.
Towards Innovative Therapies: Targeting Macrophage Subsets
The findings prompt a new therapeutic avenue—targeting specific macrophage populations. This strategy could be particularly beneficial for patients who have not responded to conventional therapies, potentially revolutionizing the management of RA.
Conclusion: A New Era in RA Research
This significant study enriches our understanding of the intricate role of macrophages in rheumatoid arthritis. By mapping distinct macrophage populations and their functional diversities, it not only elucidates their contributions to joint inflammation but also heralds new possibilities for early diagnosis and targeted therapies. As researchers continue to delve deeper into macrophage biology, patients may soon benefit from innovative approaches that could dramatically enhance treatment outcomes. Stay tuned—this could be the dawn of a new era in rheumatology!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)