Unveiling Strategies to Slash 28-Day Mortality Rates for Bacteremia Patients in Emergency Departments
2024-12-04
Author: Amelia
Study Overview
The study analyzed data from 433 patients, a near split of 49.9% females and 50.1% males, with a mean age of 74.1 years. The 28-day mortality rate was found to be a daunting 15.2%, while the 7-day mortality rate was slightly lower at 7.4%. Alarmingly, over half (59.6%) of the patients had bacteremia caused by Gram-negative bacteria, which are often more resistant to treatments. Common comorbidities among the cohort included hypertension (65.6%), type 2 diabetes (30.5%), malignancy (29.6%), and arrhythmia (23.1%).
A critical observation was the delays in antibiotic administration. On average, the time from ED admission to the first physician assessment was 1.5 hours, and it took about 10.4 hours for the initial antibiotics to be administered. Shockingly, 9.2% of patients did not receive antibiotics until over 24 hours post-admission, highlighting a potential area for improvement in patient management.
Risk Factors Uncovered
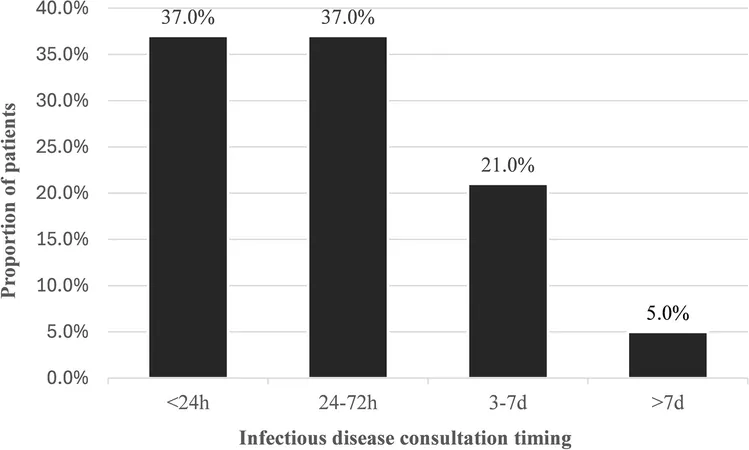
The study employed statistical analyses to identify significant factors contributing to mortality in bacteremia patients. Among the numerous associations examined, factors like age over 70, the necessity for ICU admission, pneumonia as the source of infection, and the absence of Infectious Disease (ID) consultations were found to markedly raise the risk of mortality. The risks escalate dramatically; ICU admission bears a staggering adjusted odds ratio (OR) of 6.03, marking it as the most critical predictor of poor outcomes.
By comparison, pneumonia as a bacteremia source presented nearly five times the risk of death compared to other infection origins. The researchers highlight concerns regarding hypotension—another major risk factor suggesting that timely recognition and management of this condition could save lives.
Are We Doing Enough?
The insights from this study reveal a concerning disparity in mortality rates from bacteremia compared to other acute conditions like myocardial infarction. For reference, the mortality rates for acute myocardial infarction are considerably lower, around 6.3%. There appears to be a gap in the urgency and effectiveness of treatment protocols for bacteremia.
A silver lining emerges around ID consultations, which were identified as a potentially modifiable factor to improve outcomes significantly. Past studies have shown ID consultations can decrease mortality by up to 70%, providing a crucial lifeline for patients grappling with complicated infections.
Recommendations for the Future
To curb mortality rates, healthcare systems must prioritize early ID consultations for patients presenting with bacteremia in EDs. The study emphasizes the importance of addressing the challenges faced by emergency physicians and alleviating their burdens through prompt specialists' interventions.
Furthermore, the age demographic of patients suffering from bacteremia—with over half being over 70—calls for heightened awareness and available resources to care for this vulnerable population. Clinicians should be equipped with strategies to manage hypotension and facilitate rapid diagnosis and intervention.
Concluding Thoughts
In conclusion, while the figures regarding bacteremia are grim, the study paves the way for future improvements through targeted strategies. By understanding the predictors of mortality, emergency departments can enhance patient care, optimize resource allocation and ultimately save lives. The findings serve as a clarion call for the healthcare community to address this often-overlooked condition with the urgency it demands.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)