Unveiling the Silent Struggles: Chronic Pain and Medication Use in Adults with Intellectual Disabilities
2024-12-02
Author: William
Chronic pain is one of the most pressing yet overlooked health issues facing adults with intellectual disabilities. Characterized by significant cognitive impairments, this group represents approximately 0.05% to 1.55% of the global population, depending on various diagnostic criteria and healthcare systems. Adults with intellectual disabilities often experience a range of health issues, including respiratory illnesses, poor dental health, gastrointestinal disorders, and musculoskeletal pain—conditions that are frequently painful and contribute to a reduced quality of life.
Why Are They Suffering in Silence?
The reality is that adults with intellectual disabilities not only face an increased prevalence of pain but also encounter significant barriers to effective pain management. Pain perception varies greatly, and with limited ability to articulate discomfort, many individuals do not receive appropriate care. Studies suggest that pain among individuals with intellectual disabilities is often under-recognized, leading to tragic consequences such as delayed access to healthcare, higher rates of hospitalization, and, in extreme cases, preventable deaths.
Research indicates that around 15% to 18% of adults with intellectual disabilities experience chronic pain, a figure lower than the general population's 43.5%. This disparity raises a critical question: Are healthcare professionals properly assessing and treating pain in these individuals? In many instances, they are not, largely due to the misconceptions surrounding pain thresholds and communication barriers.
The Complex Web of Medications
Alongside these health challenges, adults with intellectual disabilities are at a heightened risk of polypharmacy—the concurrent use of multiple medications—often prescribed to manage various long-term conditions. While the average individual in this demographic is prescribed approximately three medications, the risk of adverse drug reactions increases significantly, especially when considering the unique vulnerabilities of this population.
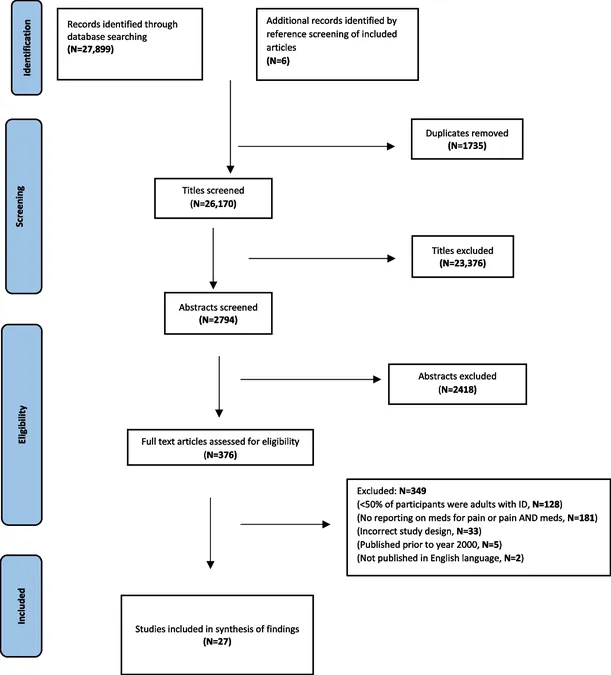
The systematic review highlighted in recent research analyzed data from nearly 28,000 references, ultimately including 27 studies—from multiple high-income countries—focused on pain-related medication in adults with intellectual disabilities. Alarmingly, findings revealed that these adults receive fewer analgesics and pain medications than those in the general population, despite having a greater prevalence of painful conditions.
Pain Management Under Scrutiny
The review delved into not only what types of analgesics are prescribed but also the influences of demographic factors and the degree of intellectual disability on medication use. Intriguingly, a disconnect exists between caregivers and the individuals they support regarding pain recognition. Caregivers often find themselves struggling to recognize pain symptoms, leading to disparities between reported pain levels and actual treatment sought.
Moreover, the findings drew attention to the tendency to prioritize psychotropic medications over pain relief medications. In some cases, this has led to behavior-management strategies that inadequately address the root causes of distress, often ignoring that the discomfort could stem from untreated pain rather than behavioral issues.
Call for Change: A Blueprint for Better Care
This comprehensive review emphasizes the urgent need for focused research to better understand pain management in adults with intellectual disabilities. Training healthcare professionals in effective pain assessment tailored to this group, advocating for policies that ensure equitable access to healthcare, and increasing overall awareness within the healthcare community are vital steps forward.
In conclusion, addressing the healthcare inequities faced by adults with intellectual disabilities, particularly regarding chronic pain, isn't just a medical need; it's a moral obligation. The findings call for a shift in how we approach pain management, aiming to ensure that every individual's suffering is acknowledged and treated with the urgency and compassion it demands.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)