A Revolutionary Discovery Brings New Hope for Patients with Inflammatory Lung Diseases!
2025-04-08
Author: John Tan
Pulmonary sarcoidosis, a debilitating lung disease marked by the presence of granulomas (tiny clusters of immune cells), has long been a source of mystery for medical professionals and patients alike. This condition is part of a broader category known as interstitial lung diseases (ILDs), all of which involve inflammation and scarring within the lungs. In the United States alone, approximately 200,000 individuals are affected by pulmonary sarcoidosis, but despite its prevalence, the underlying causes remain unknown and no new treatments have been introduced in over seven decades.
However, a groundbreaking study published in Science Translational Medicine by scientists from Scripps Research and aTyr Pharma offers promising news. Their research has identified a protein named HARSWHEP, which has the unique ability to mitigate inflammation associated with sarcoidosis by regulating white blood cells. Significantly, this reduction in inflammation not only slows disease progression but also minimizes lung scarring—long considered an irreversible consequence of this condition.
In a Phase Ib/IIa clinical trial involving efzofitimod, a therapeutic form of HARSWHEP, patients exhibited encouraging improvements. Paul Schimmel, a professor of molecular medicine and chemistry at Scripps Research and the study's senior author, remarked, “These results validate a new approach to immune regulation in chronic lung disease.” The drug functions with a gentle touch, described by Leslie A. Nangle, Vice President of Research at aTyr Pharma, as “nudging the immune system in a certain way,” rather than aggressively suppressing it. This method could halt the destructive cycle of inflammation and fibrosis that plagues patients with pulmonary sarcoidosis.
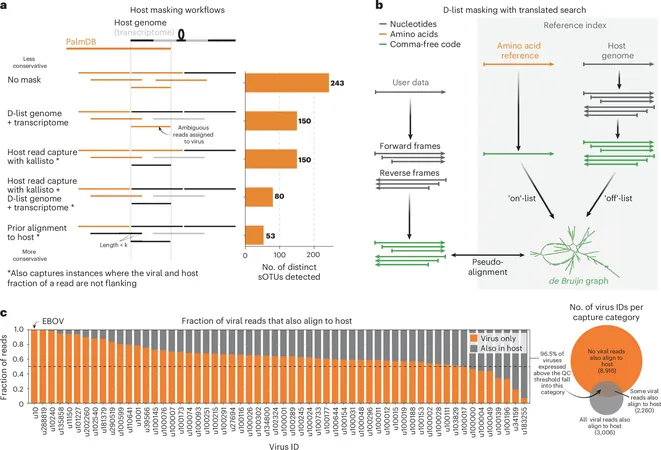
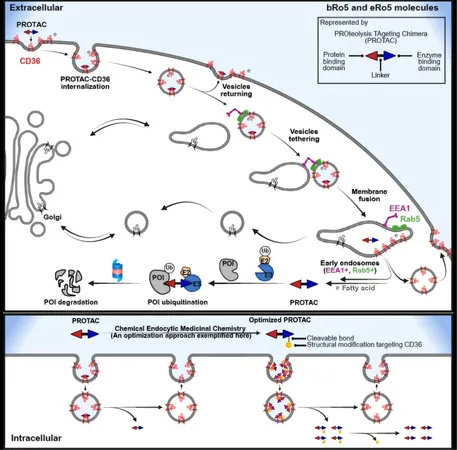
HARSWHEP belongs to a distinct class of proteins known as aminoacyl-tRNA synthetases (aaRSs), which are integral to protein synthesis in all living organisms. Over time, new variations of these proteins, known as splice variants, have evolved to interact with specific receptors on the surface of cells, inducing a range of biological responses. The team was surprised to discover that HARSWHEP binds exclusively to a receptor called neuropilin-2 (NRP2), previously associated mainly with lymphatic system development rather than direct immune responses.
Through their research, the scientists found that when monocytes (a type of white blood cell) respond to inflammation, they transform into macrophages, which then express high levels of NRP2. Nangle elaborates, “We essentially matched a protein with a newly characterized receptor implicated in immune function.” Their findings showed that HARSWHEP binding to NRP2 leads to the creation of a new macrophage type, which reduces inflammation and aids in resolving it.
In laboratory studies, administering the protein to mice and rats demonstrated reduced lung inflammation and slowed fibrosis progression. Separately, clinical trial data illustrated a positive impact on patients treated with efzofitimod while decreasing their reliance on harsh oral corticosteroids—currently the first-line treatment. Long-term corticosteroid usage is notorious for causing weight gain, organ damage, and leaving patients vulnerable to infections.
Furthermore, the researchers analyzed circulating immune cells in patients before and after efzofitimod treatment, observing a substantial decrease in inflammation indicators, including macrophage concentrations. While the focus remains on sarcoidosis, Nangle reveals that efzofitimod has the potential to treat various ILDs, with ongoing clinical trials exploring its efficacy in scleroderma-related lung disease.
This work emphasizes macrophages as a crucial target in managing ILDs and showcases the therapeutic promise of HARSWHEP—an exciting development in lung disease treatment. “This research marks the transition from concept to clinical application,” says Nangle, noting the collaboration that began in Schimmel’s lab over 15 years ago, which ultimately led to the establishment of aTyr Pharma and the clinical advancements we see today.
The emergence of HARSWHEP is not just a ray of hope for sarcoidosis patients but could potentially revolutionize treatment approaches for many other debilitating lung diseases. Stay tuned as scientists continue to unravel the mysteries of the immune system and its role in chronic illnesses!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)