Alarming Cervical Cancer Trends Uncovered: A Deep Dive into HPV Infections Among 105,679 Women in Wuhan, China
2024-10-07
Author: Arjun
Introduction
Cervical cancer, which ranks as the fourth most diagnosed cancer in women globally, poses a significant threat, accounting for over 600,000 diagnoses and approximately 342,000 deaths in 2020 alone. Shockingly, around 85% of these cases occur in low- and middle-income nations, highlighting a critical public health crisis. China is no stranger to this burden, with over 130,000 women diagnosed annually. Recent studies indicate an alarming rise in cervical cancer rates among younger populations, underlining the urgent need for effective preventive measures.
The Role of HPV in Cervical Cancer
A significant factor in this crisis is the Human Papillomavirus (HPV), a common sexually transmitted virus linked to cervical and other types of cancers. While most HPV infections resolve within two years, persistent infections can lead to various forms of cancer. Over 200 HPV genotypes have been identified, with some classified as high-risk. Notably, types 16, 18, and 58 are top culprits in cervical cancer development. Current strategies focus on prevention via vaccination and screening for precancerous lesions, which could drastically reduce incidences of cervical cancer.
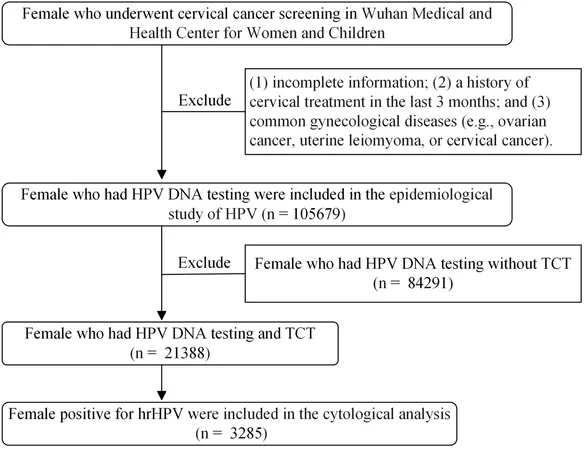
The Study
In a comprehensive research study spanning eight years, data was collected from 105,679 women screened for HPV at the Wuhan Medical and Health Center for Women and Children. This research aimed to delve into the distribution and prevalence of HPV genotypes within the region, providing vital information for vaccination initiatives and cervical cancer diagnostics.
Key Findings
The study's findings were alarming. Among participants, the overall HPV prevalence stood at 16.87%. This figure breaks down to 13.64% for high-risk HPV types, with HPV52 emerging as the most prevalent (4.24%), followed by HPV58 (2.42%) and HPV16 (2.34%). The data revealed troubling trends, with changes in HPV type prevalence over the years suggesting shifts that necessitate ongoing monitoring. Younger women (<21 years) had a notably high prevalence of HPV infections, while women aged 61-65 also showed concerning rates, emphasizing the need for targeted prevention strategies for both young and older demographics.
Implications of Findings
Statistical analyses indicated that single HPV infections predominated, although multiple infections were commonplace as well. The study further assessed the correlation between HPV types and cervical cytological conditions, revealing intricate connections between HPV presence and severity, particularly in high-grade lesions.
Factors Influencing HPV Positivity Rates
The increase in HPV positivity rates noticed in recent years could be attributed to various factors, including the expansion of cervical cancer screening initiatives in 2022 and disruptions in healthcare due to the COVID-19 pandemic. As restrictions eased, a surge in testing revealed infections that may have remained undetected during the lockdown periods.
Call to Action
Finally, insights from this vital study call for heightened awareness and action to enhance vaccination coverage and screening accessibility. With HPV vaccination having shown significant efficacy in preventing cervical cancer precursors, it is imperative for healthcare authorities to develop robust public health strategies tailored to the epidemiological characteristics of HPV across different populations.
Conclusion
As the world grapples with this pressing health issue, urgent steps must be taken to facilitate widespread HPV vaccination and effective screening. The fight against cervical cancer means acting now—will we heed the alarm?


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)