Alarming Gap in Physician Knowledge: Chronic Back Pain and Axial Spondyloarthritis Connection Exposed
2025-04-03
Author: Sarah
Introduction
A recent study conducted by Yale School of Medicine reveals a startling truth: many physicians treating chronic back pain lack the essential knowledge to accurately identify axial spondyloarthritis (AxSpA), a chronic inflammatory disorder that affects 1.4% of the population. This research, published in the esteemed Journal of Rheumatology, underscores the urgent need for greater education among healthcare professionals regarding this often-misdiagnosed condition.
The Nature of Axial Spondyloarthritis
Axial spondyloarthritis typically starts presenting symptoms in young adulthood, yet despite its prevalence, it frequently goes undiagnosed for an agonizing 8 to 14 years. Dr. Abhijeet Danve, the study's lead author and director of the Yale Spondyloarthritis Program, warns that this delay can lead to irreversible damage to the spine or sacroiliac joints, as well as impact other organ systems, elevating the risk of severe health issues like heart disease, stroke, blood clots, and hypertension.
Critical Gaps in Referrals
Dr. Danve and his team recognized a critical gap: many of the patients with chronic back pain—one of the primary symptoms of AxSpA—are not referred to rheumatologists, the specialists trained to diagnose and manage this condition. To explore this issue, they surveyed a wide range of physicians across the U.S., including family and internal medicine practitioners, spine surgeons, orthopedists, pain management professionals, and rehabilitation specialists, alongside rheumatologists.
Survey Findings
The findings from 750 physicians were telling. While 75% of the non-rheumatologists displayed knowledge of inflammatory back pain and 54% were familiar with axial spondyloarthritis, their expertise failed to translate into clinical practice. A mere 40% of these practitioners routinely assessed for the features of AxSpA, compared to nearly universal assessment among rheumatologists.
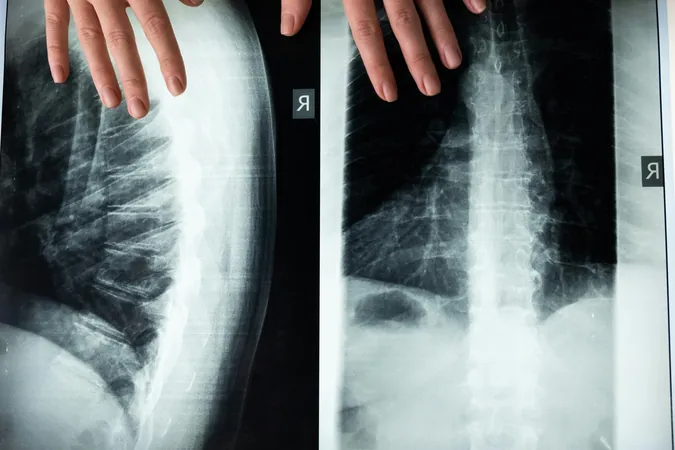
Misconceptions About Imaging Tests
One surprising revelation was the misconception surrounding the initial imaging test used to diagnose AxSpA. Dr. Danve highlighted that a pelvis X-ray is the most definitive first-step imaging needed, yet only half of the surveyed non-rheumatologists were aware of this. "If half of the physicians don't know which imaging test to order, the diagnosis will remain elusive," he warned, emphasizing the importance of timely referrals to rheumatology.
Calls for Educational Reform
The study highlights a pivotal moment for reform. Given that family and internal medicine physicians are often the first point of contact for patients and the main referral source to specialists, targeting educational efforts towards these groups could be the key to reversing the trend of misdiagnosis. Rehabilitation specialists, noted to be more aware of the pelvic X-ray recommendation, could also play an instrumental role in bridging this knowledge gap.
Conclusion
In conclusion, as the pervasive issue of chronic back pain continues to affect countless lives, there is a compelling case for enhancing physician education on axial spondyloarthritis. Without proactive measures, patients risk suffering prolonged pain and potential long-term health repercussions, stressing the urgent need for action within the medical community.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)