Alarming Rise of Crimean-Congo Haemorrhagic Fever Among Healthcare Workers in Iran (2000-2023) – A Call to Action!
2024-11-18
Author: Sarah
Introduction
Crimean-Congo haemorrhagic fever (CCHF) is a deadly viral zoonosis with a staggering case fatality rate of 5-50%. Because of the significant risk of human-to-human transmission, healthcare workers (HCWs) find themselves in particularly hazardous situations when caring for infected patients. Alarmingly, the nuances of how CCHF is transmitted among Iranian HCWs remain insufficiently understood, prompting a study aimed at revealing hidden routes of exposure over the last two decades.
Study Overview
Conducted between October 2000 and February 2023, this comprehensive examination involved 96 HCWs suspected of CCHF, who were processed at the National Reference Laboratory. Advanced testing methods like RT-PCR and IgM Capture Enzyme-Linked Immunosorbent Assay (MAC-ELISA) were utilized to confirm infections and to map exposure histories within clinical environments.
Key Findings
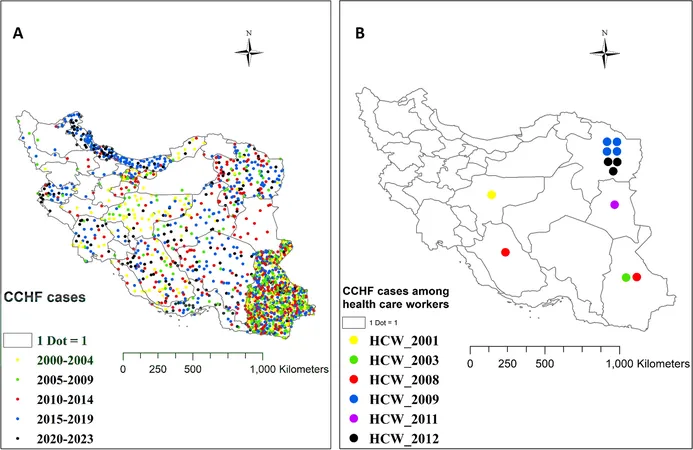
The research unearthed 12 confirmed cases of CCHF among healthcare professionals, including seven nurses and five physicians, with a median age of 32.5 years. Most notably, there was a worrying lack of direct exposure history: none reported tick bites or contact with contaminated blood or animal tissues, indicating potential gaps in safety protocols. Geographic clustering highlighted Razavi Khorasan as the most affected area, but cases also emerged from Sistan and Baluchistan, Isfahan, South Khorasan, and Fars provinces.
The predominant modes of transmission included: - Percutaneous exposure through needle sticks (3 cases) - Mucosal exposure from blood splashes (3 cases) - Skin contact with blood (3 cases) Since 2013, there have been no additional cases among HCWs, suggesting that recent safety reforms may be effective.
Transmission Patterns and Clinical Insights
The clinical presentation of CCHF featured high fever (100%), myalgia (75%), nausea, headaches, and alarming rates of thrombocytopenia and elevated liver enzymes. The incubation period ranged from 1 to 22 days, further complicating early diagnosis and treatment efforts.
Despite ribavirin being administered in most cases, treatment outcomes varied significantly, with two fatalities including a nurse and an intern, highlighting the urgency for more effective therapeutic strategies and post-exposure prophylaxis.
Conclusions and Recommendations
The results clearly show that physicians and nurses remain at high risk when caring for CCHF patients. Protective measures, including rigorous education on infection prevention and correct use of personal protective equipment, are paramount to safeguard healthcare providers from CCHF transmission.
Alarmingly, while airborne transmission remains a topic of debate, reports from this study point to potential airborne risks—one infected nurse had no direct contact with patients. This further emphasizes the need for strict adherence to safety protocols.
In addition to existing precautions, healthcare facilities should enforce comprehensive training programs focused on safe handling practices, especially for high-risk activities. With a noted seasonal pattern to CCHF cases, it is crucial to monitor healthcare settings closely during peak seasons and continue surveillance to prevent future outbreaks.
This investigation underscores a critical need for ongoing research and adaptive safety measures in a landscape where unknown risks still lurk, especially in healthcare settings. If left unchecked, the potential for CCHF to cause further devastation remains an alarming reality for healthcare providers and their patients alike!
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)