An Unexpected Diagnosis: The Surprising Case of Esophageal Tuberculosis Mimicking Cancer
2025-01-02
Author: Mei
Introduction
Esophageal ulcers can arise from both malignant and benign conditions, posing significant diagnostic challenges for healthcare providers. In an intriguing case, a 59-year-old woman presented with concerning symptoms that initially suggested esophageal cancer but were ultimately revealed to be caused by a rare condition: esophageal tuberculosis. This case highlights the importance of thorough examination and the use of advanced imaging techniques in making accurate diagnoses.
Case Presentation
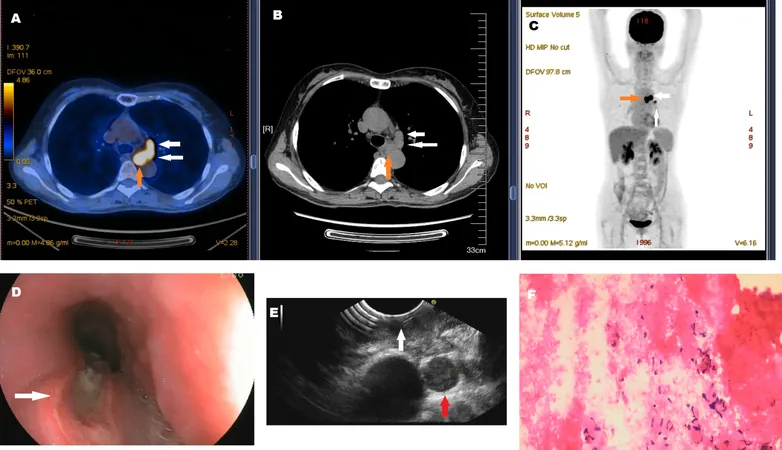
A 59-year-old female was admitted to the hospital with a month-long history of painful swallowing, general fatigue, and a notable loss of appetite. Initial assessments conducted using a whole-body 18F-FDG PET/CT scan indicated a suspicious lesion located in the mid-esophagus, accompanied by swollen mediastinal lymph nodes displaying high uptake values—an alarming indicator often associated with malignancy. The standardized uptake value (SUVmax) recorded for the lymph nodes was 17.10, while the esophageal lesion registered at 8.08, raising immediate concerns for esophageal cancer.
However, a twist in the diagnosis emerged when a biopsy performed via esophagoscopy revealed only inflammation and granulation tissue, without any malignant cells present. Further investigation through endoscopic ultrasonography was conducted, which identified caseous necrosis within the lymph nodes, and microbiological tests confirmed the presence of Mycobacterium tuberculosis. Thus, the diagnosis transitioned from esophageal cancer to esophageal tuberculosis.
Discussion
Esophageal tuberculosis is an uncommon condition that accounts for merely 2.8% of all gastrointestinal tuberculosis cases. This condition typically arises due to direct extension from nearby mediastinal lymph nodes rather than originating from pulmonary tuberculosis. The clinical presentation of esophageal tuberculosis closely resembles that of esophageal carcinoma, which often leads to misdiagnosis.
In this case, despite the absence of typical tuberculosis symptoms such as fever and weight loss, the patient's positive tuberculin skin test indicated exposure to the bacteria, reinforcing the significance of thorough differential diagnosis. As confirmed by studies, both PET/CT imaging and endoscopy are critical in identifying esophageal lesions and differentiating between malignant and benign conditions.
Given the potential for misdiagnosis, medical professionals are urged to adopt endoscopic techniques like endoscopic ultrasonography, which can boast a sensitivity and specificity rate of approximately 95-98% in distinguishing between tumor types.
Remarkably, following an intensive four-month regimen of antituberculous chemotherapy, including rifapentine and moxifloxacin, the patient showed significant improvement with resolution of symptoms, esophageal ulcer, and the enlarged lymph nodes.
Conclusion
This case serves as an essential reminder in the medical community about the importance of differentiating between esophageal malignancies and benign conditions like tuberculosis. The overlap in clinical presentations can easily lead to errors, making advanced imaging and biopsy critical components of modern diagnosis. As medical technology continues to evolve, the accuracy and effectiveness of patient diagnoses improve, ultimately leading to better outcomes and fewer invasive procedures. When faced with an esophageal lesion, a comprehensive approach that includes endoscopy and imaging is paramount in ensuring that patients receive the appropriate care they need.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)