Breakthrough in Appendicitis Management: New Predictive Model Could Save Lives!
2024-10-09
Author: John Tan
Introduction to Acute Appendicitis
Acute appendicitis (AA) is a prevalent surgical emergency worldwide, impacting nearly 100 out of every 100,000 adults annually. Most cases occur in individuals aged 20 to 40, with a lifetime risk of developing appendicitis estimated at 7-8%. Appendicitis can be classified into uncomplicated and complex forms, where complex appendicitis, which includes instances of gangrene or perforation, accounts for around 30% of cases in the U.S. This serious condition is associated with a heightened risk of complications, such as peritonitis and septic shock, significantly raising mortality rates when compared to uncomplicated appendicitis.
Current Treatment Approaches
Typically, treatment for appendicitis is an appendectomy supplemented by antibiotics. The growing preference for laparoscopic appendectomy is tempered by concerns over surgical risks, costs, and complicated recovery times, prompting a reevaluation of treatment strategies that prioritize patient safety. Notably, some patients have undergone unnecessary appendectomies, resulting in negative pathology reports.
Antibiotic Treatment for Uncomplicated Appendicitis
Recent investigations underscore the viability of antibiotic treatment alone for uncomplicated appendicitis. However, in cases of gangrenous or perforated appendicitis (GPA), the risk of treatment failure is alarming, often leading to severe complications. Due to this, timely surgical intervention remains critical, with early identification of GPA essential for guiding treatment decisions.
Limitations of Existing Scoring Models
Despite existing scoring models for predicting complex appendicitis, most lack robustness, relying on limited variables and single-center data. Our study aims to rectify this by developing a novel scoring system that accounts for radiographic findings, laboratory results, and clinical parameters, specifically aimed at predicting GPA and enhancing clinical decision-making.
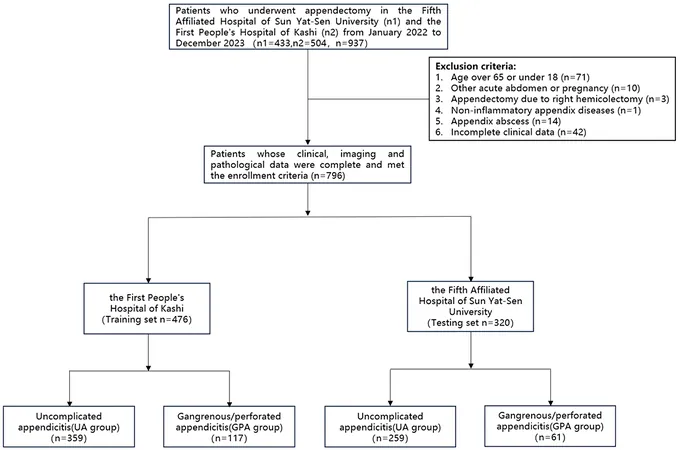
Development of the Predictive Model
Over 900 patients who underwent appendectomy within a two-year period were analyzed across two hospitals to create a reliable predictive model. By applying logistic regression to a carefully curated cohort, we developed a scoring tool with a focus on objective data, including blood test results and CT scan findings. Among evaluated factors, specific laboratory markers such as white blood cell count, lymphocyte levels, D-dimer, blood glucose, and albumin, as well as CT indications of appendix size and the presence of fecalith, showed a strong correlation with GPA.
Validation and Clinical Implications
Our findings demonstrated a robust predictive capacity with an accuracy rate of 70.6% and sensitivity of 82.1% in identifying patients at risk of GPA. Validation of this model across a diverse patient population confirmed its clinical utility, further underscoring its potential to aid in timely surgical management.
Advantages of the New Scoring Model
This new scoring model transcends previous limitations by integrating data from multiple hospitals, reinforcing its applicability in varied clinical settings. The implications of this research are profound; by adopting a structured approach to identifying high-risk appendicitis patients, healthcare providers can effectively streamline treatment protocols, potentially reducing morbidity and mortality associated with delayed surgical intervention.
Future Directions
Further research is essential to refine this model, explore its applicability in older populations, and ensure its effectiveness across broader demographics. By addressing the challenges of complex appendicitis management with innovative tools, we can aspire to significantly improve surgical outcomes and prioritize patient care.
Conclusion
Will this predictive model revolutionize appendicitis treatment? Stay tuned for more groundbreaking medical insights!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)