Breakthrough in Heart Care: First-Line Catheter Ablation Outperforms Drugs for Post-Heart Attack Patients!
2024-11-16
Author: Li
Breakthrough in Heart Care: First-Line Catheter Ablation Outperforms Drugs for Post-Heart Attack Patients!
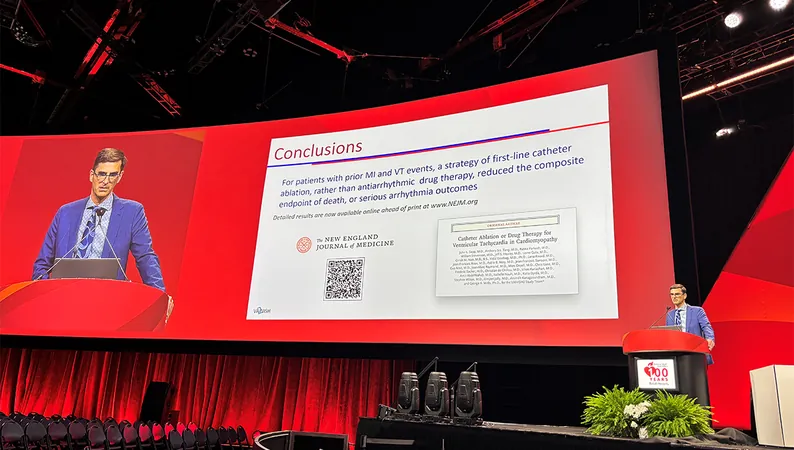
In a groundbreaking revelation presented at the 2024 American Heart Association (AHA) Scientific Sessions in Chicago, a recent study known as the VANISH2 trial has found that catheter ablation for patients with ischemic cardiomyopathy and ventricular tachycardia (VT) may be significantly more effective as a first-line treatment than conventional antiarrhythmic drugs. This study offers compelling evidence for a shift in treatment strategies for patients who have experienced a heart attack and have an implantable cardioverter-defibrillator (ICD).
Lead author Dr. John Sapp from the QEII Health Science Center in Halifax, Canada, stated during the presentation that catheter ablation resulted in better outcomes regarding death and severe arrhythmia, a game-changing finding for managing this high-risk patient population. The findings were concurrently published in the prestigious New England Journal of Medicine.
Patients with VT post-myocardial infarction (MI) often suffer from recurrent tachycardia which can severely impair their quality of life and survival rates. Although ICDs are effective at treating VT episodes through painful shocks, the prospect of alternative therapies, such as catheter ablation, offers new hope for patient recovery and wellness. Sapp highlighted that previous research has already suggested a preference for ablation when antiarrhythmic treatments fail, making this trial essential for understanding the benefits of ablation when used as the first-line treatment option.
In the VANISH2 study, researchers analyzed data from 416 participants (predominantly male, median age 68) who had a history of heart attack, were equipped with an ICD, and were experiencing clinically significant VT. They were randomly assigned to either receive catheter ablation within two weeks or undergo antiarrhythmic drug treatments with sotalol or amiodarone, with a median follow-up of 4.3 years.
Results from this expansive study revealed that patients who underwent catheter ablation experienced significantly fewer composite adverse outcomes compared to those treated with medications—50.7% versus 60.6%, respectively. The decline in treated sustained VT, driven below the detection threshold of the ICDs after treatment, was particularly noteworthy, underscoring the procedure's effectiveness.
Dr. Sana Al-Khatib, who moderated the press conference, expressed excitement at the prospects of integrating earlier interventions like catheter ablation into treatment protocols. She emphasized the need for reevaluating long-standing practices of delaying ablative therapies for patients suffering from ICD shocks.
Moreover, the study noted that the timing of catheter ablation is crucial and should be considered earlier in the treatment pathway rather than as a last resort. Other trials, including PAUSE-SCD, PREVENTIVE-VT, SMASH-VT, and VTACH, have similarly supported the notion that early ablation could prove beneficial even before ICD implantation.
The adverse effects observed from catheter ablation included two fatalities and various nonfatal events, such as strokes and vascular injuries. While the antiarrhythmic medications presented high numbers of side effects, including respiratory issues and gastrointestinal complications, the risk profile could indicate the need for personalized treatment strategies that prioritize effective yet safe management options.
Notably, the trial included a minimal representation of female participants, a phenomenon identified in many clinical trials. Dr. Sapp theorized that this may stem from gender-related differences in heart attack timing and incidence, resulting in fewer women presenting with post-MI VT during the study period.
The findings from VANISH2 are not just academic; they could transform the standard of care for patients suffering from VT following heart attacks. As discussant Dr. Usha Tedrow of Brigham and Women’s Hospital stated, the experience of painful ICD shocks underscores the urgency for more effective treatments, reinforcing the appeal of catheter ablation as a promising solution.
With a growing body of evidence pointing to the advantages of earlier intervention strategies like catheter ablation, the landscape of cardiac care is poised for significant change, improving not only survival rates but also the quality of life for countless patients battling the dangerous repercussions of traumatic heart events.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)