Breakthrough in Nanotechnology: Targeted Lipid Nanoparticles Cross the Blood-Brain Barrier to Treat Neurodegenerative Diseases!
2024-12-18
Author: Li
Breakthrough in Nanotechnology: Targeted Lipid Nanoparticles Cross the Blood-Brain Barrier to Treat Neurodegenerative Diseases!
In an exciting development, Penn Engineers have taken a revolutionary leap in nanotechnology by modifying lipid nanoparticles (LNPs)—the same technology that made waves during the COVID-19 pandemic with mRNA vaccines. These enhanced LNPs now demonstrate the ability to not only traverse the notoriously difficult blood-brain barrier (BBB) but also pinpoint specific cell types, including neurons. This innovative advance could pave the way for groundbreaking treatments for neurological disorders such as Alzheimer’s and Parkinson’s diseases.
In their recent publication in Nano Letters, the researchers introduced a novel method using peptides—short chains of amino acids—that act as precise targeting molecules. This allows LNPs to deliver mRNA directly to endothelial cells lining the blood vessels in the brain, as well as to the neurons themselves. This ability to target cells specifically is crucial because effective treatments for neurodegenerative conditions must ensure that mRNA reaches the right location within the brain.
According to Michael J. Mitchell, an Associate Professor in Bioengineering and senior author of the paper, this is a significant enhancement of previous efforts. He likens the earlier stage of their research to sending a package across the country without knowing its final destination. “With peptides, we can now address the package to specific destinations, much like sending to every house with a red mailbox,” he explained.
Understanding the Challenge of the Blood-Brain Barrier
The BBB serves as a protective shield, evolved to block unwanted molecules, including various drugs, from entering the brain. This barrier is highly selective, actively expelling substances deemed hazardous. While some treatments can be directly injected into the brain, these procedures are invasive and not always feasible.
Interestingly, the BBB is permeable to fat-soluble substances—like alcohol and THC—which is where the lipid composition of these nanoparticles provides an advantage. Certain formulations of LNPs, made from fatty compounds found in common oils, can adeptly bypass the BBB, allowing for potential therapeutic interventions directly in the brain.
Peptides vs. Antibodies: A Game-Changer
Historically, most research targeting specific organs with LNPs has involved antibodies—large proteins that function like biological address labels. However, this approach has notable downsides, as attaching antibodies can destabilize the LNPs and increase their size, complicating their passage through the BBB.
Peptides, in contrast, are significantly smaller (typically just dozens of amino acids long), making them easier and cost-effective to attach in large quantities to LNPs. Moreover, they present a lower risk of aggregation, which can interfere with formulation and compromise efficacy.
The inspiration for using peptides arose serendipitously. Emily Han, the paper’s first author, shared how an unexpected encounter with a bat prompted her to investigate rabies vaccines, leading her to discover RVG29. This promising molecule is a 29-amino-acid segment of the glycoprotein from the rabies virus, known for its ability to cross the BBB.
Rigorous Testing to Validate Efficacy
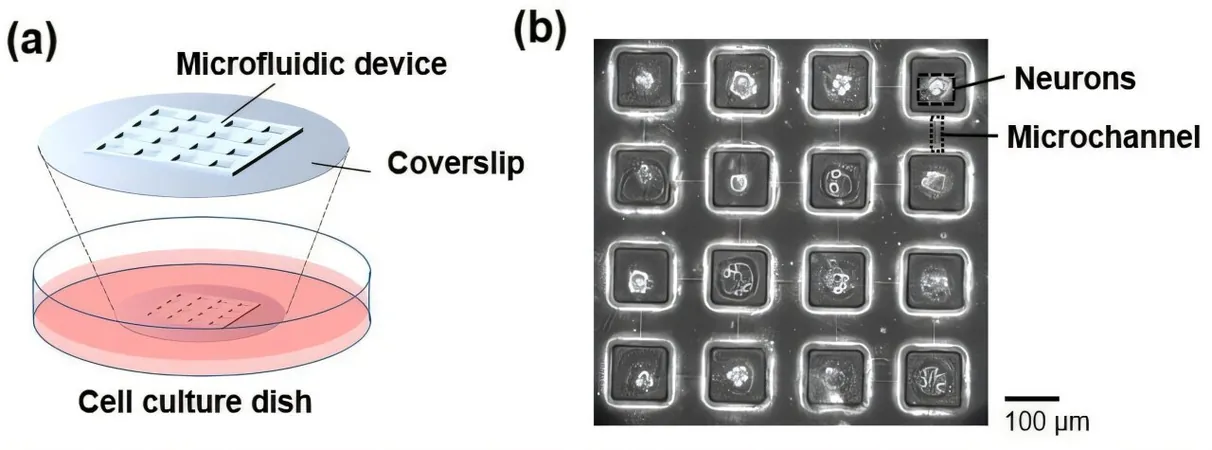
The team began their validation process by ensuring that the peptides adhered effectively to the LNPs. “Our LNPs consist of a complex mixture of nucleic acids, lipids, and peptides,” Han noted. They meticulously optimized their quantification methods to distinguish peptide signals from the complex backdrop.
After confirming attachment, the next challenge was to assess whether these peptide-functionalized LNPs (pLNPs) reached their targets in animal models. Mapping cellular activity in the brain is difficult because of the diverse cell types and the presence of fat that can cloud measurements. For over six months, Han honed a meticulous protocol to analyze brain tissue, akin to a mechanic disassembling an engine for repairs.
Looking Ahead: The Future of Neurological Treatments
The research team is now focused on determining the extent of neuron treatment necessary with pLNPs to produce meaningful clinical outcomes. “Do we need to treat every neuron, or would reaching 10% suffice to alleviate symptoms?” Mitchell questioned.
Answers to these inquiries will guide the refinement of delivery strategies, bringing the vision of mRNA-based treatments for Alzheimer’s, Parkinson’s, and other debilitating brain diseases closer than ever before. The implications of this research are not only exciting but carry the potential to fundamentally change the treatment landscape for millions suffering from neurodegenerative conditions.
With these advances in nanoparticle technology, the future of medicine looks promising, and we may soon be able to achieve what was once thought impossible — targeted, effective treatment for some of the toughest neurological diseases out there!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)