Breakthrough in Osteosarcoma Research: Machine Learning Reveals Key Subtypes for Tailored Treatments!
2024-12-23
Author: Mei
Groundbreaking Study Uncovers Osteosarcoma Subtypes
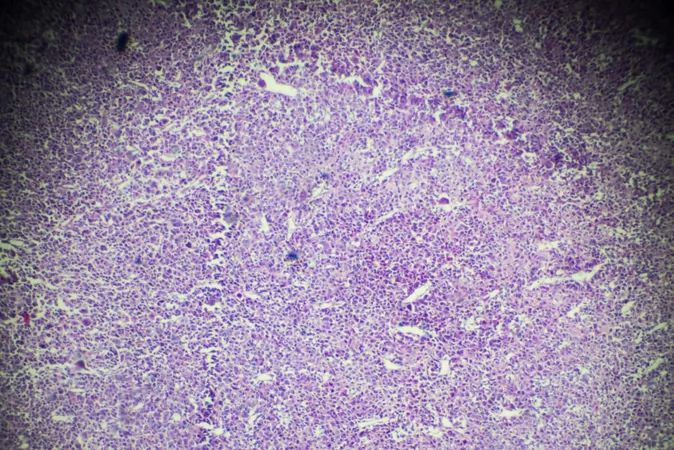
A groundbreaking study conducted by researchers at the University of East Anglia (UEA) has unlocked the potential to revolutionize the treatment of osteosarcoma—an aggressive and rare type of bone cancer primarily affecting children and teenagers. Leveraging the power of machine learning, the team has successfully identified at least three distinct subtypes of osteosarcoma, promising a new era for more personalized and effective medical interventions.
Machine Learning Technology
Funded by Children with Cancer UK, the research, which has been published in Briefings in Bioinformatics, employs a sophisticated machine learning technique known as Latent Process Decomposition (LPD). This advanced model analyzes genetic data and allows for precise categorization of patients based on the unique characteristics of their tumors. This could notably enhance the efficacy of clinical trials and overall patient treatment strategies.
History of Treatment Approaches
Historically, osteosarcoma has been mostly treated with a one-size-fits-all approach involving chemotherapy and surgery. However, this method has often led to suboptimal responses, leaving many patients with limited treatment options and severe side effects. Dr. Darrell Green, the lead author of the study and a lecturer at UEA Norwich Medical School, emphasized the inadequacies of past treatment modalities by stating, 'Since the 1970s, osteosarcoma has been treated using untargeted chemotherapy and surgery, which sometimes results in limb amputation as well as the severe and lifelong side effects of the chemotherapy.'
Clinical Trial Challenges
The complexity and heterogeneity of osteosarcoma have historically posed significant challenges for clinical trials. Many trials have been deemed unsuccessful due to a low response rate to new therapies. However, the discoveries from this latest research suggest that the failures may have been misinterpreted. Green remarked, 'The new medicines were not a total ‘failure’... they could have become a new treatment for select patient groups.'
Identifying Critical Functional States
By utilizing the LPD model, researchers identified critical 'functional states' within tumors. This groundbreaking approach not only recognizes the differences within individual tumors but also paves the way for more accurate matching of treatments to specific disease subtypes. The model revealed one subtype that displayed a notably poor response to the standard chemotherapy regimen, MAP (methotrexate, doxorubicin, and cisplatin).
Biomarkers for Future Diagnostics
As a significant advancement, the research also pinpointed a set of eight genes consistently dysregulated in osteosarcoma, which could serve as biomarkers for future diagnostics. These genes may aid in recognizing high-risk patients and informing more strategic treatment decisions.
Limitations and Future Directions
While the findings are promising, the researchers acknowledge some limitations, particularly the small dataset on which the model was developed. However, they express optimism that the model will evolve as more comprehensive data becomes available.
Implications for Clinical Trials
The identification of osteosarcoma subtypes sparks hope for reshaping the clinical trial landscape. By improving how patients are stratified based on genetic expression, there is a greater likelihood of success for new drugs. Currently, the survival rate for osteosarcoma remains around 50%, holding steady for the past 45 years. Researchers advocate for future clinical trials to group patients by their cancer subtype to tailor treatments effectively. Dr. Green and his colleagues anticipate that these innovations in diagnostic labeling and stratified treatment will lead to significantly enhanced survival rates for osteosarcoma in the future.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)