Breakthrough in Schizophrenia Research: Understanding Disease Processes in Nerve Cells
2024-12-16
Author: Jia
Breakthrough in Schizophrenia Research: Understanding Disease Processes in Nerve Cells
In a groundbreaking study, researchers from the NMI Natural and Medical Sciences Institute in Reutlingen have made significant strides in understanding the complex mechanisms behind schizophrenia, a mental health disorder that has long been treated primarily through symptom management. This new knowledge opens the door for the potential development of innovative treatment options targeting the root causes of the illness. The findings have been shared in the prestigious journal BMC Psychiatry.
The importance of proteins cannot be overstated in biological systems; they are essential for a multitude of processes. When proteins are misfolded or malfunction, it can lead to serious health issues, including schizophrenia, where neuronal development is severely affected.
Uncovering the Early Signs of Schizophrenia
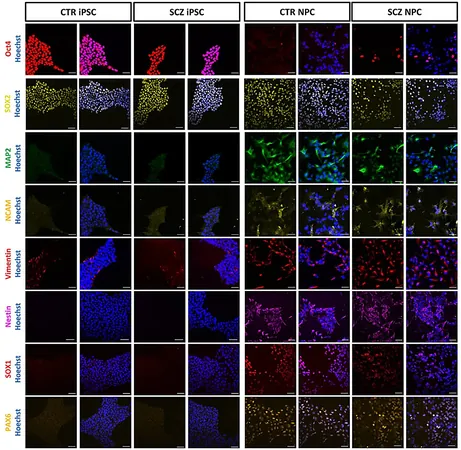
Led by researchers Aaron Stahl, Prof. Hansjürgen Volkmer, and Dr. Markus Templin, the NMI team utilized cutting-edge DigiWest technology to conduct a meticulous analysis of neuronal cells derived from patients. These cells, sourced from the University Hospital of Tübingen, provided a comparative framework between affected and healthy individuals, paving the way for early identification of the molecular failures linked to schizophrenia.
Stahl commented, "By observing neurons in their early developmental stages, we have identified that abnormal cells lag in their development, and crucially, we understand *why* this occurs." This early insight may revolutionize the approach to diagnosing and intervening in the disorder.
What the Research Reveals About Schizophrenia
The team's analysis revealed critical information regarding the dysfunction of cellular processes within neurons afflicted by schizophrenia. The research spotlighted specific malfunctions, including defects in DNA repair mechanisms and irregularities in cell cycle regulation—the latter being a fundamental process that ensures proper cell division.
Moreover, alterations in the p53 regulatory pathway were noted. This protein plays a vital role in controlling cell growth and can lead to serious diseases such as cancer when improperly regulated. The investigation suggests a strong correlation between these dysfunctional processes in neurons and the onset of schizophrenia.
Dr. Templin expressed optimism about their findings: "Our protein analyses have significantly enhanced our understanding of the triggers associated with schizophrenia. This is a monumental step toward developing targeted medical therapies that tackle the disease at its origin." However, he cautioned that while progress has been made, it may still take considerable time before these insights translate into effective treatments.
The implications of this research are profound. For the millions of individuals affected by schizophrenia worldwide, this study not only sheds light on the underlying biological mechanisms of their condition but also signals hope for future innovations in the treatment landscape. As researchers continue to untangle the complexities of mental health disorders, a closer look at the cellular processes involved could one day lead to groundbreaking therapeutics that transform lives.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)