Breakthrough Study: Can Coronary Artery Calcium Scores Transform Heart Disease Prevention and Statin Prescriptions?
2025-03-31
Author: Jia
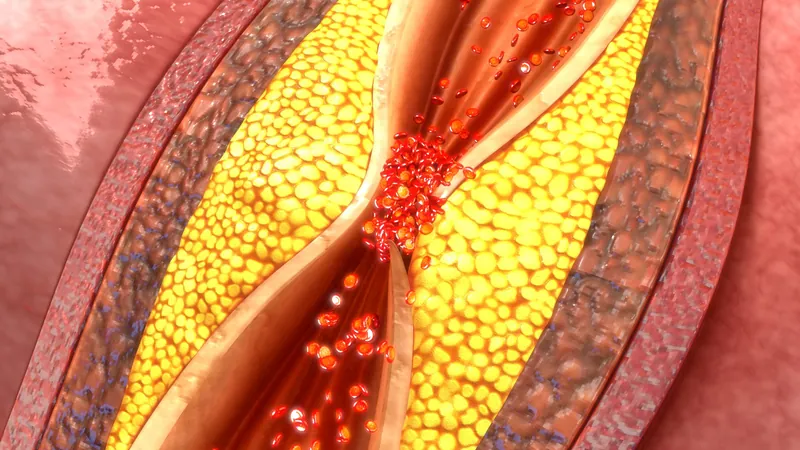
Recent research from Intermountain Health in Salt Lake City has unveiled a game-changing method for assessing heart disease risk: coronary artery calcium (CAC) scores, derived from a non-invasive CT scan. This innovative approach not only predicts the likelihood of developing coronary artery disease (CAD) within five years but may also reshape the landscape of statin prescriptions, potentially reducing unnecessary medication use.
The study presented at the latest American College of Cardiology conference revealed that a zero CAC score—indicative of no detectable plaque in the coronary arteries—correlates with a significantly lower risk of premature death. "Individuals with a zero-plaque burden not only show a low risk of heart disease but also experience two to three times lower mortality rates from any cause," remarked Dr. Jeffrey L. Anderson, the study's lead investigator.
The CAC score is determined through a CT scan that uses X-rays to identify calcium deposits in the coronary arteries, an early indicator of plaque buildup. The scoring system ranges from zero, which represents no advanced plaque, to higher scores indicating increasing plaque presence, thus allowing doctors to intervene before serious complications, like heart attacks, occur.
The CorCal Outcomes trial, which is an extensive retrospective study analyzing data from 40,820 symptomatic patients over a decade, utilized PET/CT scanning to quantify calcified plaques. Alarmingly, only 0.12% of patients under 65 and 0.25% of those over 65 with a CAC score of zero faced coronary events, underscoring the score's predictive power.
Dr. Anderson further emphasized the importance of CAC scores in assessing overall health: "A zero CAC score might suggest not only an exceptionally low risk of coronary death but also a decreased likelihood of death from other causes, as vascular health often reflects the state of other organs."
The implications for statin prescriptions are substantial. Traditionally, doctors have relied on risk factors such as age, cholesterol levels, and smoking history to recommend statins, often leading to over-prescription. In the study, nearly half (50.7%) of patients evaluated using conventional risk factors received statin recommendations, compared to only 22.3% for those assessed with CAC scores. This discrepancy points to a more tailored, data-driven approach for determining who truly needs these cholesterol-lowering medications, particularly among older patients who may not have significant coronary artery disease.
As the CorCal Outcomes study progresses towards its completion in 2026, researchers will continue to investigate the long-term effectiveness of different methods for statin prescription, monitoring key outcomes such as heart attacks and stroke rates. "The upcoming years are critical for understanding how these new insights can improve patient outcomes,” stated Dr. Anderson.
On the broader front, this research could significantly alter clinical practices. By emphasizing individualized assessments through CAC scores, healthcare providers could better identify individuals at high risk for heart disease while also minimizing unnecessary prescriptions of statins, ultimately sparing patients from potential side effects and unnecessary costs.
Furthermore, the researchers are set to explore how the correlation between a zero CAC score and overall health extends to other vascular diseases and potentially even cancer connections. What this means for the future of cardiovascular health could be revolutionary, allowing for earlier, more precise interventions that not only add years to lives but also life to years.
Stay tuned as we await the profound implications of this groundbreaking study that could reshape the strategies we use to combat heart disease!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)