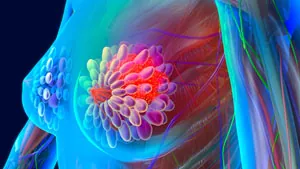
Breakthrough Study Reveals: Many Patients with Intermediate-Risk Breast Cancer Can Skip Chest Wall Irradiation Post-Mastectomy!
2024-12-13
Author: Arjun
Groundbreaking Study Presentation
In a groundbreaking revelation presented at the 2024 San Antonio Breast Cancer Symposium, researchers have found that patients with intermediate-risk breast cancer may not need to undergo chest wall irradiation after a mastectomy, challenging longstanding medical conventions.
Research Leadership and Trial Background
Dr. Ian Kunkler from the University of Edinburgh led this pivotal research, derived from the BIG 2-04 MRC SUPREMO clinical trial. The findings indicate that there is no significant difference in 10-year overall survival rates for patients who received chest wall irradiation compared to those who did not. Specifically, 81.4% of patients who underwent irradiation were alive after nearly a decade, closely aligning with the 82.0% survival rate of their non-irradiated counterparts.
Historical Context of Chest Wall Irradiation
Historically, postmastectomy chest wall irradiation has been the gold standard for patients with early-stage breast cancer, particularly those with four or more positive axillary lymph nodes. However, Dr. Kunkler emphasizes that the necessity of this treatment for patients with fewer positive lymph nodes—one to three, or even those with no positive nodes—remains a topic of debate.
Defining Intermediate-Risk Patients
The study categorized intermediate-risk breast cancer patients as those possessing one to three positive lymph nodes or those with node-negative disease that exhibited higher-risk features, such as aggressive cancer cell types or lymphovascular invasion. The clinical trial involved an extensive participant pool of 1,607 patients across multiple countries, underscoring the international significance of this research.
Local Recurrence Reduction
While it was confirmed that chest wall irradiation substantially curtails the risk of local recurrence by more than 50%, the absolute reduction in recurrence was less than 2%, which Dr. Kunkler described as a "clinically insignificant" improvement in outcomes.
Implications for Patient-Clinician Interactions
The implications of this study are significant for patient-clinician interactions and decision-making processes regarding cancer treatment plans. The data suggest that many patients might be eligible to forgo the additional radiation therapy post-surgery without compromising their long-term survival rates.
Acknowledging Limitations
Despite the promising findings, researchers acknowledged limitations, including the low number of patients with larger tumors (pT3, N0 disease) and the unexpectedly high overall survival rates in the studied groups.
Encouraging Patient Engagement
As clinical practices evolve based on this emerging evidence, patients should engage in open discussions with their healthcare providers to tailor treatment plans that align with their specific cancer profiles and preferences. This research not only enhances our understanding of breast cancer management but also empowers patients with crucial information about their treatment options in the fight against this pervasive disease.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)