Breakthrough Therapy Unveiled for Deadly Glioblastoma — Hope on the Horizon?
2024-10-07
Author: Rajesh
Glioblastoma (GBM) is an insidious brain tumor notorious for its lethal nature, boasting a median survival rate of only 12-16 months following diagnosis. Astonishingly, the two-year survival rate for patients grappling with GBM plummets to under 10%.
Specialists have long faced two substantial hurdles in battling GBM: the difficulty of anti-tumor drugs penetrating the blood-brain barrier effectively and the swift development of resistance by GBM cells to conventional treatments. However, a groundbreaking study from The Ohio State University Comprehensive Cancer Center presents potential hope in the fight against this formidable foe.
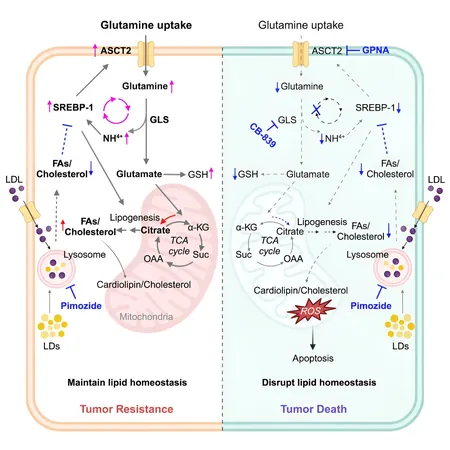
In a remarkable discovery, lead researcher Deliang Guo, Ph.D., a prominent figure at the OSUCCC and professor at The Ohio State University College of Medicine, highlighted the benefits of combining an unconventional brain-penetrating antipsychotic drug, pimozide, with a cutting-edge glutamine metabolism inhibitor known as CB-839. This innovative combination not only appears to combat tumor resistance but also effectively stymies GBM growth.
The research findings, now published in the prestigious journal Cell Reports Medicine, are built on an extensive analysis involving 223 glioma patient samples, unveiling an uncharted connection between the glutamine transporter ASCT2 protein and a noteworthy lipogenic regulator, SREBP-1. Further validation of this mechanistic link was carried out using preclinical mouse models, yielding significant insights.
Researchers found that GBM cells tend to simultaneously boost their glutamine intake and lipid production, which fuels their accelerated growth. Guo explained that pimozide plays a pivotal role in inhibiting the release of cholesterol and fatty acids from cellular lipid stores, thereby starving tumor cells of essential building blocks. However, the study revealed that, on its own, pimozide failed to deliver optimal results against GBM.
This resistance stems from GBM's ability to upregulate its glutamine uptake and consumption, a challenge that the research team is keenly aware of. Nonetheless, they are optimistic that their findings will resonate across diverse fields such as cancer biology, metabolism, and treatment methodologies.
Co-first author Yaogang Zhong, Ph.D., anticipates that this innovative therapeutic strategy might not only be revolutionary for glioblastoma but could extend its benefits to various other cancers that are similarly dependent on glutamine and lipids.
Collaborators on this vital research included Ohio State's College of Pharmacy, Department of Biomedical Informatics, Translational Data Analytics Institute, and partnered institutions like the University of Louisville and University Clermont Auvergne in France.
As we stand on the brink of potentially transformative advances in glioblastoma treatment, future studies will be essential to determine the full impact of this combination therapy. Patients and medical professionals alike may soon have reason to hope as this remarkable research enters the next phase of clinical trials. Will this blend of unconventional drugs redefine the future of glioblastoma treatment? Only time will tell, but the promise is indeed tantalizing.





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)