
Breast Cancer in 2024: A Reflection on the Past and a Vision for the Future
2024-11-08
Author: Siti
In an insightful review featured in The New York Times, author Barron Lerner revisited Betty Ford’s 1974 breast cancer diagnosis, a pivotal moment in the history of breast cancer treatments. Far from being merely a personal crisis, Ford's diagnosis instigated a national dialogue about breast cancer awareness and significantly increased the adoption of screening practices across the United States. However, it is important to note that Ford's cancer was not identified through screening and was node-positive, which raises questions about the effectiveness of early detection methods in preventing mortality.
As we reflect on the past 50 years since Betty Ford’s diagnosis, it is imperative to evaluate how our understanding of breast cancer screening and treatment has evolved. The conventional narrative surrounding cancer progression and the benefits of early detection may need reexamination.
The Evolving Landscape of Breast Cancer Treatment
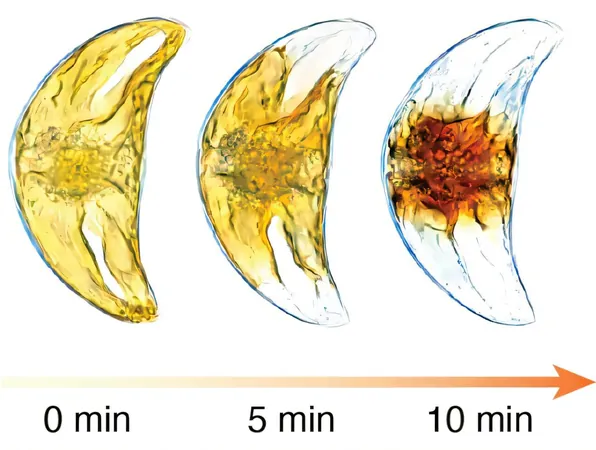
Historically, the goal of breast cancer screening has been to catch cancers while they are small and node-negative, with the assumption that smaller cancers yield better survival rates. While it's commonly believed that larger tumors pose a higher threat, new research suggests that even small tumors can carry similar risks as their larger counterparts. Current data indicates that women diagnosed with tumors measuring just 1 cm may have comparable survival rates to those with even smaller tumors, challenging long-standing beliefs about cancer size and its implications for prognosis.
Betty Ford's lymph node-positive cancer calls attention to the reality that mammographic screening is designed to detect smaller tumors, but not specifically those that have already spread to the lymph nodes. Data from the Women’s College Hospital indicates that reductions in tumor size correlate with improved mortality rates, but the question remains: does mammography reliably benefit patients by identifying node-positive cancers?
One of the most significant studies in the last half-century, led by Bernie Fisher, demonstrated that survival rates for breast cancer patients are similar whether they undergo lumpectomy or radical mastectomy. Even with fewer recurrences in mastectomy patients, this notable finding from 1991 shows that surgery alone does not dictate outcomes when it comes to mortality.
Rethinking Conventional Wisdom
Research indicates that invasive cancer development following treatment can still result in a positive prognosis. A striking point from recent studies is that women with ductal carcinoma in situ (DCIS) experience similar survival rates regardless of whether they undergo mastectomy or lumpectomy, undermining the belief that more aggressive surgery equates to better outcomes.
Furthermore, the Canadian National Breast Screening study, of which I was a senior author, randomly assigned participants to yearly mammograms or physical exams. Over 30 years, breast cancer mortality in both groups remained nearly equal. Despite facing substantial criticism, particularly from the radiology community, the study reinforced the idea that early detection via mammography may not confer a significant benefit in terms of life-saving outcomes.
The Future Outlook: Prioritizing Research and Understanding
Much of the progress seen in breast cancer mortality rates over the past decades can be credited to advancements in chemotherapy, which have improved survival outcomes. The majority of women diagnosed today—particularly those with node-positive cancers—can often achieve long-term remission without chemotherapy or extensive surgery. Research indicates that lymph node and distant metastases might stem from separate cellular origins, suggesting the necessity for a fresh perspective on how we approach breast cancer treatment.
As we enter 2024, the focus of breast cancer research should shift towards understanding the earliest stages of cancer development and determining the sources of rogue cells that lead to metastasis. While screening plays a role for some, it highlights the pressing need to adopt new strategies that get us closer to eliminating this perilous disease. We may be on the cusp of a new paradigm where prevention and early intervention take a more sophisticated and individualized approach, ultimately aiming for a breast cancer mortality rate that continues to decline.
Conclusion
Assessing the legacy of Betty Ford illustrates a multifaceted history of breast cancer awareness, treatment, and survival. As we evolve, so too must our strategies for detection, treatment, and ultimately, prevention of breast cancer in future generations.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)