Can the Femoral Vein Replace the Inferior Vena Cava in Volume Assessment for Chest Pain Patients?
2024-11-28
Author: Wei
Introduction
In emergency departments, assessing a patient’s volume status is critical, especially for those presenting with chest pain. Traditionally, ultrasound measurement of the inferior vena cava (IVC) diameter has been utilized for this purpose, indicating intravascular fluid volume. This method, however, is not without limitations; factors like cardiac function, respiratory fluctuations, and intra-abdominal pressures can affect IVC measurements. As such, the femoral vein (FV) has emerged as a prospective alternative due to its accessibility and potential reliability in situations where the IVC cannot be adequately visualized.
Study Overview
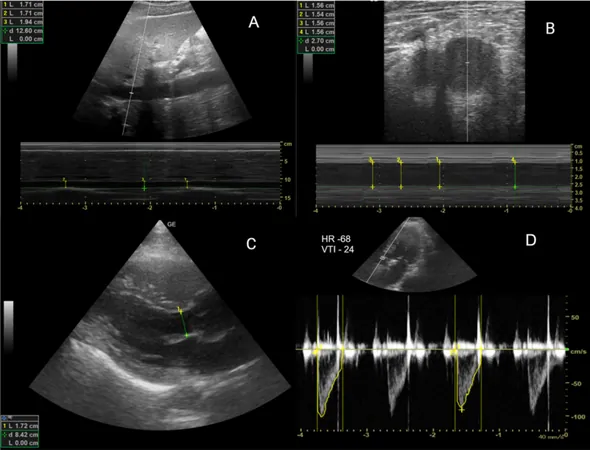
In a groundbreaking single-center study conducted at a tertiary care hospital in southern India, researchers evaluated the correlation between IVC and femoral vein collapsibility indices in a cohort of 85 patients experiencing chest pain. Employing point-of-care ultrasound, both IVC and FV diameters were measured to identify their effectiveness in assessing fluid responsiveness. Measurements were conducted before and after a passive leg-raising (PLR) maneuver, a technique previously recognized for its role in evaluating patients’ volume status.
Results and Findings
The study revealed that while both IVC and FV diameters significantly increased after the PLR test, there was insufficient correlation between their collapsibility indices. The results indicated no significant relationship between these indices and cardiac output, which raises questions about their effectiveness as reliable indicators of fluid responsiveness in this patient group.
Further analysis using standard statistical methods demonstrated that although post-PLR measurements reflected changes consistent with intravascular volume expansion, the findings suggested that neither IVC nor FV metrics could be deemed accurate substitutes in this context. This disparity may be attributed to structural differences between the two veins and their physiological responses to position changes.
Clinical Implications
Volume resuscitation is a cornerstone in the management of critically ill patients, with accurate monitoring of fluid status essential for preventing complications such as pulmonary edema and multi-organ dysfunction. The inability to rely solely on either the IVC or FV indices suggests a necessity for a more integrated approach to volume assessment.
Exploring Future Directions
With the limitations of this study acknowledged, including a small sample size and a homogenous patient profile, the authors advocate for larger-scale investigations. These studies should encompass diverse clinical populations to better understand the utility of the femoral vein in volume assessment beyond the context of stable patients experiencing chest pain.
While preliminary insights into the femoral vein’s suitability for fluid responsiveness assessment are intriguing, the need for further research is clear. Integrating various strategies, including the use of echocardiography, could enhance the precision of volume evaluations in emergency care settings. The findings serve as a clarion call for clinical practitioners to reconsider current protocols in favor of methodologies that ensure patient safety, optimize outcomes, and develop more nuanced approaches to critical care.
Conclusion
As emergency clinicians navigate the complexities of fluid volume assessment, the insights gained from this study signal a pivotal consideration: understanding the distinct behaviors of the inferior vena cava and femoral vein is vital. The quest for the most reliable methods in a high-stakes environment continues, emphasizing the need for robust, conclusive studies that pave the way for enhanced patient management in emergency and critical settings.
Stay tuned as we unravel more about emerging medical techniques that could revolutionize emergency care!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)