Convalescent Plasma Could Have Saved Hundreds of Thousands During COVID-19 Crisis!
2024-10-03
Introduction
A groundbreaking study from the Johns Hopkins Bloomberg School of Public Health reveals that the widespread use of convalescent plasma during the COVID-19 pandemic could have potentially saved hundreds of thousands of lives, particularly among high-risk outpatients and newly admitted hospitalized patients.
What is Convalescent Plasma?
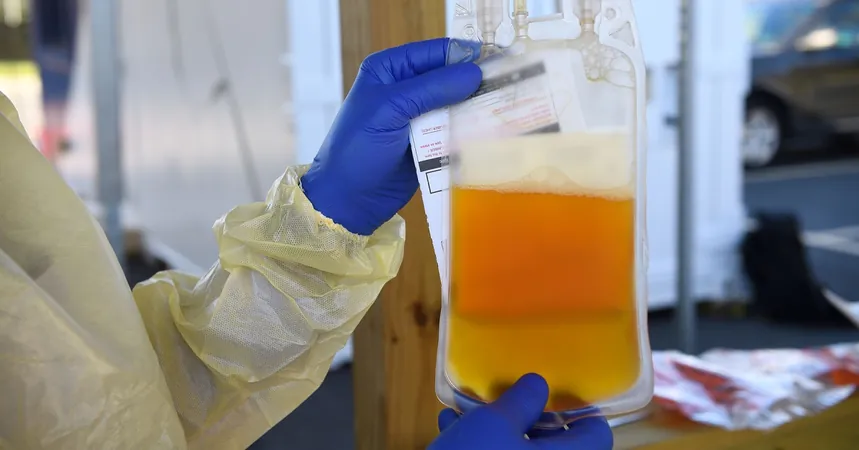
Convalescent plasma, a therapy involving blood plasma from individuals who have recovered from the infection, was implemented in the early stages of the pandemic. This treatment utilizes the antibodies present in the plasma, which can help to neutralize the virus and potentially lessen the severity of the disease in others—a concept that has shown effectiveness in past pandemics, including the 1918 influenza pandemic and the SARS outbreak in the early 2000s.
Study Findings
During the first year of the COVID-19 pandemic alone, over 500,000 patients in the U.S. received this treatment. According to the study published in the Proceedings of the National Academy of Sciences on October 1, researchers estimate that administering convalescent plasma could have saved between 16,476 and 66,296 lives for hospitalized patients during a critical period from July 2020 to March 2021. This estimate is based on comprehensive data analyses, including weekly mortality and usage statistics.
Potential Impact of Early Administration
The potential life-saving impact of convalescent plasma was even greater under optimistic scenarios. If 100% of hospitalized COVID patients had received high-titer convalescent plasma promptly after admission, researchers estimate that between 37,467 to 149,318 lives could have been saved—up to a staggering 125% increase in survival rates.
Outpatient Treatment Benefits
Interestingly, the research showed how significant changes in outpatient treatment could have further reduced hospitalizations. For instance, if merely 15% of outpatients had received convalescent plasma, between 85,268 and 227,377 hospitalizations could have been avoided. The numbers become even more impressive—up to 1.1 million avoided hospitalizations—if more than three-quarters of outpatients had been treated.
Limitations of Current Approval
Despite its promise, convalescent plasma was initially approved only for hospitalized patients, a limitation that researchers argue hampered its potential impact. Casadevall, a leading expert and advocate for the use of convalescent plasma, pointed out earlier studies showed mixed results largely due to critical timing—the therapy was often administered too late in the disease progression to be effective. However, subsequent clinical trials indicated that early administration could significantly decrease the risk of hospitalization.
Safety and Cost
The safety profile of convalescent plasma is reassuring, with treatments costing around $750 per unit—less expensive than many novel COVID-19 therapies.
Call to Action
The researchers urge public health authorities to incorporate the use of convalescent plasma into future emergency preparedness plans. The logistical frameworks and established protocols already exist; thus, setting up outpatient centers for early intervention should be a priority for managing future infectious disease outbreaks.
Conclusion
However, the study does acknowledge some limitations, including uncertainties about the exact number of convalescent plasma units administered and variability in efficacy across different clinical settings.
“Preparedness for future pandemics requires active measures to harness proven therapies like convalescent plasma,” stated Casadevall. “We can and should have systems in place to treat patients early, utilizing established medical knowledge without needing new technology.”
As we reflect on the lessons learned during the pandemic, the proactive use of convalescent plasma stands out as a crucial strategy that could have dramatically altered the course of this global health crisis.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)