Dapagliflozin: A Game-Changer for Heart and Kidney Health in Diabetics Undergoing Heart Procedures?
2025-04-26
Author: Arjun
Unlocking the Benefits of Dapagliflozin in Diabetic Patients
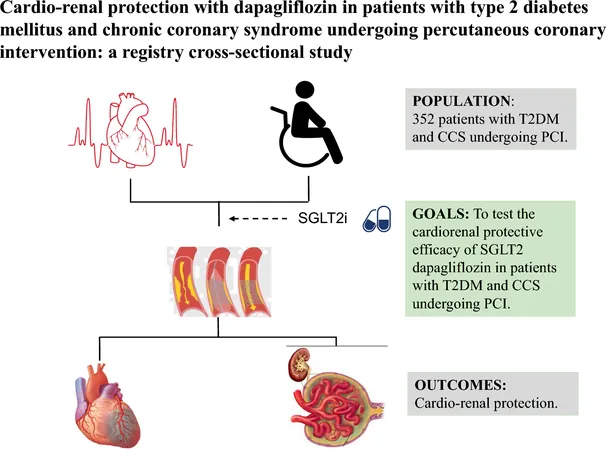
A groundbreaking registry study has revealed exciting insights into the effects of dapagliflozin—a medication typically used to manage type 2 diabetes mellitus (T2DM)—on patients with chronic coronary syndrome (CCS) during percutaneous coronary interventions (PCI). This research, conducted at Beijing Hospital between 2018 and 2021, analyzes data from inpatients diagnosed with T2DM and CCS, exploring how dapagliflozin impacts both cardiac and renal outcomes.
Who Was Included in the Study?
The study focused on inpatients aged 18 and older, ensuring they had complete medical records. Eligible patients had to have documented use of dapagliflozin for more than seven days before their PCI, while those without SGLT2 inhibitors were included as a control group. Key exclusions were made for patients suffering from severe heart disease, significant allergies, or incomplete medical records.
What Were the Key Findings?
The results painted a compelling picture. Firstly, dapagliflozin significantly improved cardiac outcomes, with lower rates of periprocedural myocardial infarction (PMI) observed among those treated with the medication. Notably, this effect persisted even after adjusting for various clinical variables.
When it came to renal outcomes, the drug did not significantly reduce the rate of contrast-induced acute kidney injury (CI-AKI). However, subgroup analyses showed benefits for older patients (65+), those with multivessel disease, and individuals receiving high contrast volumes. Furthermore, the dapagliflozin group demonstrated better kidney function, as evidenced by higher estimated glomerular filtration rates (eGFR) both before and after PCI.
Why Is Myocardial Protection Important?
Myocardial injury is a leading cause of complications following cardiac procedures. Dapagliflozin's ability to reduce PMI events highlights its potential as a protective measure against heart damage during PCI. The study's findings suggest that starting dapagliflozin more than a week prior to procedures may enhance cardiovascular benefits, especially for high-risk populations.
Renal Injury: A Double-Edged Sword?
Contrast agents used in PCI pose a risk for renal impairment, making renal protection vital. While dapagliflozin didn’t show a significant impact on CI-AKI compared to controls, it did contribute to a more stable eGFR trajectory. This suggests that early dapagliflozin use may help mitigate rapid declines in kidney function post-PCI.
What Challenges Remain?
Despite these promising results, the study's retrospective nature means caution is warranted. The relatively small sample size from a single center limits the generalizability of findings, and long-term outcomes remain unexplored. Future studies should aim for larger, multi-center cohorts to confirm dapagliflozin's protective effects on the heart and kidneys in T2DM and CCS patients.
Conclusion: A Potential Breakthrough?
This pioneering research may herald a new era in diabetes care, emphasizing the systemic benefits of dapagliflozin beyond glucose control. As we continue to unravel its cardioprotective and renoprotective properties, dapagliflozin might just be the key to enhancing outcomes for patients battling both diabetes and coronary heart disease.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)