Evaluating Vaccination Strategies Against the Mpox Outbreak in NYC: Insights and Recommendations
2024-09-30
Author: Yu
Background
Since May 2022, the mpox virus has led to alarming outbreaks in various countries, prompting health authorities to focus on vaccination as a primary method of control. Yet, challenges such as vaccine shortages and diminishing efficacy continue to pose significant hurdles in the effective management of the disease, making decisions regarding vaccine allocation increasingly critical.
Methods
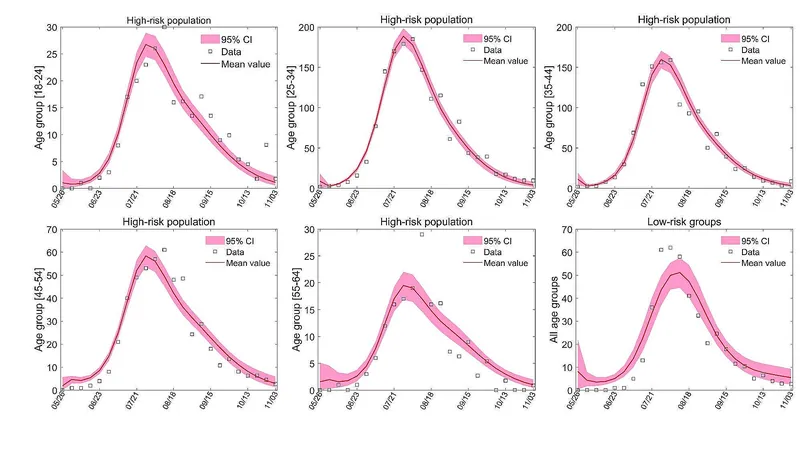
In an effort to assess the situation in New York City, researchers developed an advanced epidemiological model that tracked the prevalence of mpox using surveillance data from May 19 to November 3, 2022. This model aims to simulate various vaccination scenarios—both with and without pre-pandemic vaccinations—to better understand the potential outcomes of different strategies.
Results
The findings indicate an alarming potential rise in new infections: without vaccination, cases could swell by approximately 385%, extending the transmission period by around 350%. Conversely, initiating vaccinations before the outbreak could reduce the number of new infections by as much as 96%, underscoring the proactive role of vaccination in controlling epidemics.
Notably, the mpox outbreak in New York is believed to have been exacerbated by the Pride events, highlighting the dynamic nature of transmission during mass gatherings. However, the study suggests that even if a similar event occurs in the future, the current vaccination coverage should prevent large-scale outbreaks.
Key Facts about Mpox
The mpox virus, an orthopox virus akin to smallpox, poses severe health risks, including rashes and serious symptoms like swollen lymph nodes and even death in desperate cases. Historically, 97% of those infected will develop visible symptoms, yet the disease is largely self-limiting. The virus was first recognized in 1958 but gained traction in human populations when cases were identified in the 1970s. As of November 2022, global infections surged to over 73,000 across 108 countries, with the U.S. reporting the highest case load.
The infection spreads primarily through human-to-human contact, particularly among men who have sex with men, highlighting specific demographics at heightened risk. Current protective measures appear inadequate, especially for those born post-1980 who have never been vaccinated against smallpox, which provides significant, albeit waning, immunity to mpox.
Model Structure and Surveillance Data
The model employed categorized the population into high-risk and low-risk groups based on age and sexual behavior, capturing the complexity of susceptibility among varied demographic cohorts. This segmentation enables more precise modeling of disease dynamics in response to intervention strategies. Surveillance data was drawn from New York City health reports to reflect real-time cases and vaccination progress.
Calibrating and Analyzing the Model
Using state-of-the-art statistical methods such as Markov Chain Monte Carlo (MCMC), researchers honed the model to align with observed trends, allowing for accurate predictions of the epidemic's trajectory. The effective reproduction number (R_e) was calculated to assess transmissibility, revealing that the outbreak peaked amidst the heightened contacts at the Pride event.
Conclusion and Recommendations
The urgency of effective vaccination strategies has never been more pronounced. This research advocates for prioritizing vaccinations among high-risk groups between the ages of 34 and 45, who display a greater propensity for infection, thereby mitigating the spread of mpox.
Even with a slight increase in cases as global travel resumes, the findings support the notion that, with continued vaccination efforts, New York City can avoid another catastrophic outbreak akin to that of 2022. Thus, proactive vaccination—including the timely provision of smallpox vaccines—remains a necessary strategy to combat the mpox crisis effectively.
Healthcare authorities must remain vigilant, adapting strategies as needed to ensure community protection and public health security in the face of evolving viral threats.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)