Groundbreaking Discovery Unveils Mechanism Behind Breast Cancer Progression and Treatment Resistance
2024-12-09
Author: Wei Ling
Groundbreaking Discovery Unveils Mechanism Behind Breast Cancer Progression and Treatment Resistance
A monumental breakthrough in breast cancer research has revealed a crucial mechanism that drives both cancer invasion and drug resistance, shedding light on one of the most challenging aspects of oncology.
University of Liverpool Findings
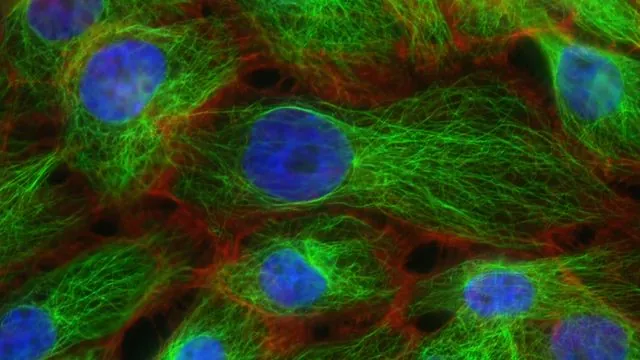
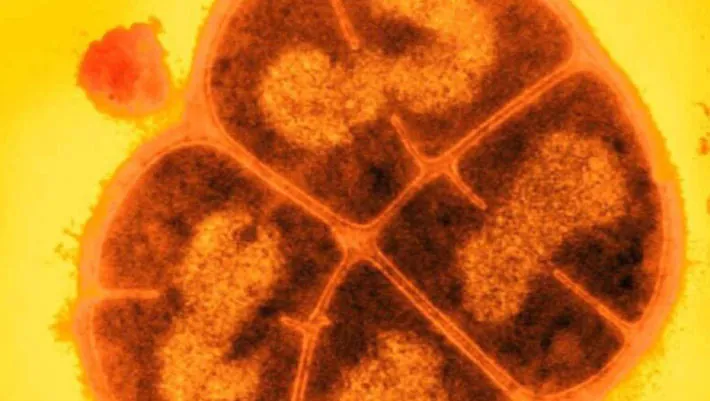
Recent findings from a study conducted by researchers at the University of Liverpool focus on ‘HER2-positive’ breast cancer, noted for its aggressive nature. This particular form of breast cancer has two significant molecules—HER2 and αVβ6 integrin—that not only independently predict patient outcomes but also interact in a complex ‘crosstalk’ mechanism responsible for facilitating cancer cell invasion.
Molecular Interactions and Drug Resistance
The study unveils that when αVβ6 integrin is activated, it recruits HER2 along with a molecular network encompassing RAB5, RAB7A, and GDI2. This complex communication system enhances the movement and signaling capabilities of HER2 and αVβ6 within cancer cells, promoting invasive behavior. More critically, the research indicates that in cases where breast cancer cells develop resistance to trastuzumab—a widely used treatment for HER2-positive breast cancer—this network is fundamentally disrupted. The loss of GDI2, a pivotal regulator within this interaction circle, diminishes the effectiveness of therapies aimed at blocking HER2 or αVβ6, enabling the cancer to exploit alternative invasion pathways and thus become more aggressive and harder to treat.
Implications for Patient Outcomes
A remarkable aspect of this study is the implication of these molecular interactions on patient outcomes. Elevated levels of GDI2 correspond with improved survival rates. In contradiction, increased expression of αVβ6 indicates a higher risk of relapse after trastuzumab treatment, highlighting its potential as a biomarker for determining patients at greater risk of therapeutic failure. This finding may lead to more refined treatment strategies tailored to individual patient needs.
Expert Commentary
Lead researcher Dr. Mark Morgan emphasizes the significance of these discoveries, stating, "Understanding how breast cancer invades tissue and becomes resistant to treatments is crucial. The identification of this αVβ6-HER2 interaction opens promising new pathways for innovative treatment interventions."
Future Directions
The researchers propose that targeting the RAB5/RAB7A/GDI2 regulatory module or restoring its normal functioning could aid in preventing or delaying the emergence of resistance in HER2-positive breast cancers. Regular monitoring of αVβ6 levels in patients may also serve as a predictive tool for treatment outcomes, informing more personalized therapeutic approaches.
Community Response
Dr. Simon Vincent from Breast Cancer Now reinforces the importance of this research. He states, "Drug resistance is one of the greatest hurdles we face in breast cancer treatment. Comprehending the mechanisms behind resistance will ensure that patients have multiple treatment options available, thereby increasing the chances of successful outcomes."
Conclusion
Looking ahead, the researchers aim to explore the development of targeted therapies that can specifically attack cells with high αVβ6 expression, potentially improving survival rates and offering new hope for patients battling this aggressive cancer type. This study not only enhances our understanding of HER2-positive breast cancer progression but also maps out a path towards tackling one of the most critical barriers in cancer treatment today.
In light of these findings, the push for more research and funding into treatment innovations remains paramount, as the fight against breast cancer continues to progress against the backdrop of its formidable complexities.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)