Groundbreaking Discovery: Why Cancer Immunotherapy May Leave Patients Vulnerable to Infections
2024-11-27
Author: Ming
Groundbreaking Discovery: Why Cancer Immunotherapy May Leave Patients Vulnerable to Infections
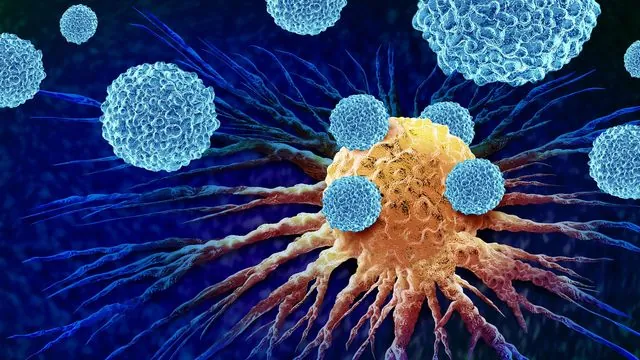
Recent research from a multinational collaboration, spearheaded by the Garvan Institute of Medical Research, has unveiled a startling reason why cancer patients undergoing immunotherapy with checkpoint inhibitors are at a heightened risk for common infections. This pivotal study, published in the journal *Immunity*, offers new insights into the immune system's response, setting the stage for preventative measures against this concerning side effect of cancer treatment.
Professor Stuart Tangye, co-senior author of the study and head of the Immunology and Immunodeficiency Lab at Garvan, explained that although immune checkpoint inhibitors have revolutionized cancer therapy by empowering T cells to combat tumors more effectively, approximately 20% of patients still face an increased incidence of infections—an issue that has remained poorly understood until now.
“Our findings indicate that while checkpoint inhibitors significantly enhance anti-cancer immunity, they simultaneously impair B cells, the very components of our immune system tasked with producing antibodies that protect against infections,” says Professor Tangye. This discovery represents a crucial step toward understanding and mitigating the adverse effects associated with immunotherapy.
The research honed in on PD-1, a molecular target that acts as a 'brake' on the immune system, preventing excessive T cell activity. The therapeutic promise of checkpoint inhibitors comes from their ability to release this brake, thereby unleashing a more robust immune attack on cancer. However, the study’s findings reveal that this activation can inadvertently hamper the ability of B cells to function effectively.
In collaboration with researchers from Rockefeller University and Kyoto University Graduate School of Medicine, the team examined patients with rare genetic deficiencies of PD-1 or its partner PD-L1, alongside animal models. They discovered a significant link: impaired PD-1 signaling led to a diminished diversity and quality of antibodies produced by memory B cells—crucial cells responsible for ‘remembering’ and responding to past infections.
Dr. Masato Ogishi, the study’s first author from Rockefeller University, stated, “Individuals with a genetic deficiency in PD-1 or PD-L1 exhibited reduced antibody diversity and fewer memory B cells, making it increasingly difficult for their immune systems to mount effective responses against common pathogens.”
Dr. Kenji Chamoto from Kyoto University elaborated on the dual nature of PD-1 inhibition, describing it as having a 'yin and yang' quality; while it bolsters anti-tumor immunity, it simultaneously detracts from B-cell defenses. This duality highlights a delicate balance inherent in immune homeostasis.
The implications of this research underscore the necessity for clinicians to vigilantly monitor B cell functionality in patients receiving checkpoint inhibitors. Dr. Stéphanie Boisson-Dupuis from Rockefeller University emphasized the importance of recognizing the delicate trade-off: enhanced anti-cancer effects could come at the cost of the immune system’s ability to fend off infections.
One promising intervention emerging from these findings is immunoglobulin replacement therapy (IgRT), a treatment designed to replace missing antibodies in patients with immune deficiencies. The research advocates for considering IgRT as a preventative measure for cancer patients deemed at elevated risk for infections.
“Studying rare genetic conditions such as PD-1 or PD-L1 deficiency grants us invaluable insights into normal immune function and the potential consequences of manipulating it,” reflected Professor Tangye. “This research paves the way for refining immunotherapies to maximize their therapeutic benefits while minimizing harmful side effects.”
Looking ahead, the research team plans to delve deeper into methods to enhance checkpoint inhibitor therapies, striving to retain their potent anti-cancer effects while safeguarding patients’ immune defenses.
This groundbreaking study showcases the integral relationship between cancer research, genomics, and immunology, offering hope for future innovations that could dramatically improve patient outcomes across the globe.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)