Groundbreaking Research Reveals How Early Gut Microbes Can Shield Against Diabetes
2025-01-04
Author: Wei
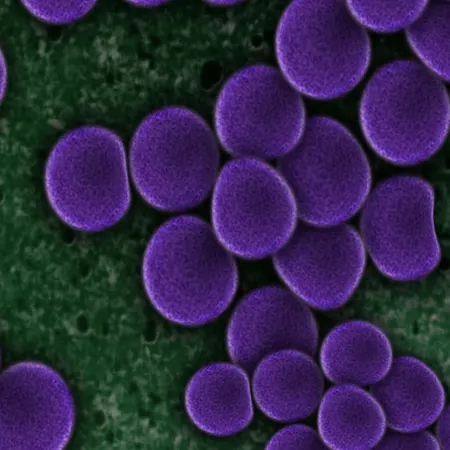
Recent studies on mice have unveiled fascinating insights into the role of gut microbes during early life and their potential to significantly influence metabolic health, particularly in the prevention of type 1 diabetes. Researchers found that the composition of the microbiome during infancy shapes the development of insulin-producing beta cells, which are crucial for regulating blood sugar levels throughout life.
A Race Against Time: The Critical Window for Microbial Influence
In a compelling discovery, scientists demonstrated that mice treated with broad-spectrum antibiotics shortly after birth exhibited detrimental long-term effects on metabolic health. Those mice developed a notably reduced number of beta cells, along with elevated blood sugar levels and diminished insulin production by the time they reached adulthood. Lead researcher June Round, a professor at the University of Utah Health, expressed concern over the findings, stating, "It showed how important the microbiota is during this very short early period of development."
Unlocking the Power of Specific Microbes
The study went further by testing various antibiotics, allowing researchers to identify specific gut microbes that enhanced insulin production and improved metabolic function. Notably, the fungus *Candida dubliniensis*, which is rarely studied and absent in healthy adult humans, showed promise as a beneficial organism present in infants.
Remarkably, when genetically predisposed male mice received this fungus early in life, their chances of developing type 1 diabetes plummeted from a staggering 90% to less than 15%. This protection was echoed when researchers introduced the fungus to adult mice that had lost their insulin-producing cells—leading to regeneration of these critical cells and restored metabolic function.
Potential Implications for Human Health
If these promising results translate to human health, microbiome-derived treatments might eventually restore pancreatic function in individuals battling diabetes. However, Jennifer Hill, who spearheaded the study, underscores the challenges, noting that therapies successful in mice often fail to yield similar outcomes for humans.
The Link Between Microbes and Immune Function
The role of *C. dubliniensis* in supporting pancreatic health seems intertwined with immune system functionality. Previous studies have established that pancreatic immune cells can promote the health of neighboring insulin-producing cells. Notably, mice devoid of a microbiome exhibited a decrease in these vital immune cells, further exacerbating metabolic dysfunction. However, when these mice received *C. dubliniensis* in their early development, both their immune response and metabolic health improved significantly.
The researchers believe that there are likely many other beneficial microbes yet to be discovered that could confer similar protective effects against diabetes, indicating a vast, largely uncharted landscape in microbiome research.
Looking Ahead: A Future of Microbe-Based Diabetes Prevention
The implications of this research extend beyond basic understanding, hinting at the possibility of preventive strategies that could alter the course of diabetes before it starts. As Round optimistically stated, "What I hope will eventually happen is that we're going to identify these important microbes and we'll be able to give them to infants so that we can perhaps prevent this disease from happening altogether."
In an era where the complexities of the human microbiome are becoming more evident, this research highlights the enormous potential for early intervention strategies aimed at fostering a healthier future—one where the specter of diabetes can be diminished through the power of tiny microorganisms. Stay tuned as we uncover more about these microbial heroes and how they may revolutionize our approach to health and disease prevention!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)