Groundbreaking Research Uses Tumor-Derived Organoids to Personalize CAR-T Cell Therapy for Glioblastoma Patients
2024-12-09
Author: Nur
Introduction
In a revolutionary study, researchers from the Perelman School of Medicine at the University of Pennsylvania have successfully created organoids from the tumors of glioblastoma (GBM) patients, using these models to track responses to CAR-T cell therapy in real time. This unprecedented approach could represent a significant breakthrough in the personalized treatment of one of the most aggressive forms of brain cancer.
Understanding Glioblastoma and CAR-T Cell Therapy
Glioblastoma is notorious for its complexity and resilience, often resulting in a bleak prognosis, with patients typically surviving just 12 to 18 months after diagnosis. While conventional treatments—like surgery, radiation, and chemotherapy—have shown limited efficacy, CAR-T cell therapy has emerged as a promising option. This therapy works by reprogramming a patient’s T cells to seek and destroy specific cancer cells; however, it has faced hurdles in effectively targeting solid tumors like GBM.
Research Methodology and Findings
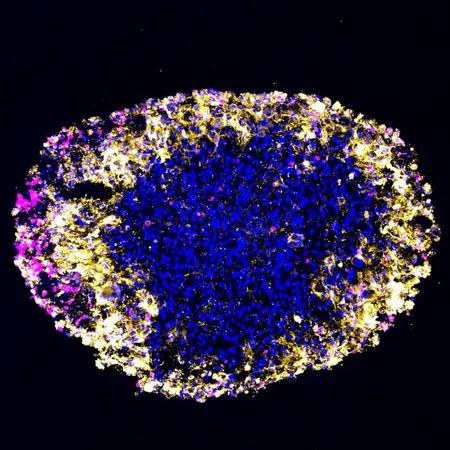
In this study, the researchers focused on patients with recurrent GBM who participated in a Phase I clinical trial for a dual-target CAR-T cell therapy. By cultivating organoids from their tumors post-surgery, the team was able to conduct parallel experiments, treating the organoids concurrently with the patients. Remarkably, the results showed that the organoids mirrored the patients' responses. If the tumors in the organoids shrank after treatment, the same was true for the tumors in the patients’ brains.
The Significance of Organoids
Professor Hongjun Song emphasized the significance of this development, stating, 'Measuring a GBM patient's response to treatment is challenging due to the difficulties in performing regular biopsies on the brain.' This research could drastically enhance personalized treatment plans by providing insights into individual tumor behaviors.
Published Findings
The findings were documented in a paper published in Cell Stem Cell, where the authors highlighted that this is the first-ever clinical trial that implements patient-matched organoid studies that align seamlessly with patient treatment timelines.
What Makes This Approach Unique?
The organoids provide a “living” model that reflects the intricate complexity of the tumor microenvironment—something previous models have struggled to replicate. The study co-senior author, Dr. Guo-li Ming, explained that existing tumor models often lack the diversity of cancer cells and their interactions with surrounding tissues. By studying patient-derived organoids, the researchers can observe how tumors react to therapies in a more realistic setting.
Future Implications
This research not only helps in understanding patient-specific tumor responses but also lays the groundwork for future clinical applications. The team hopes that in the future, organoids could be utilized to identify optimal treatment pathways for individual patients before actual therapy starts.
Impact on Treatment Strategies
One of the alarming aspects of CAR-T cell therapy for GBM is the risk of neurotoxicity, which can cause significant complications. Surprisingly, the findings from the organoids also mirrored the cytokine responses seen in the patients’ cerebrospinal fluid, highlighting that these models can give predictions about side effects as well.
Expert Insights
Dr. Donald M. O’Rourke, a co-senior author on the study, remarked, 'Our GBM organoids serve as a powerful tool to dissect the intricacies of how CAR-T cell therapy interacts with brain tumors.' The hope is that these models will not only personalize patient care but also enhance overall understanding of how to combat this formidable cancer.
Conclusion
By demonstrating strong correlations between organoid responses and patient outcomes, this pioneering research could catalyze further investigations into personalized therapies for glioblastoma. The ultimate aim is to leverage these organoids to test a variety of treatment options swiftly, potentially selecting the best CAR-T therapies or novel drugs available. In conclusion, the preliminary success of this research establishes a hopeful avenue for future treatments. If organoid technology continues to advance, it may hold the key to improving survival rates among glioblastoma patients who desperately need innovative and effective treatment options. The fight against this deadly disease may finally be entering a new era—one where personalized medicine reigns supreme.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)