
India’s Groundbreaking Initiative: Thousands of Medics Mobilized to Eradicate Cervical Cancer with HPV Vaccine
2025-04-01
Author: Li
In an ambitious effort to eliminate cervical cancer, India is training tens of thousands of healthcare professionals to advocate for the human papillomavirus (HPV) vaccine. This lifesaving initiative aims to empower mothers during medical visits to ensure they consider vaccinating their daughters, while also taking education to schools and community centers to combat rampant misinformation about vaccines.
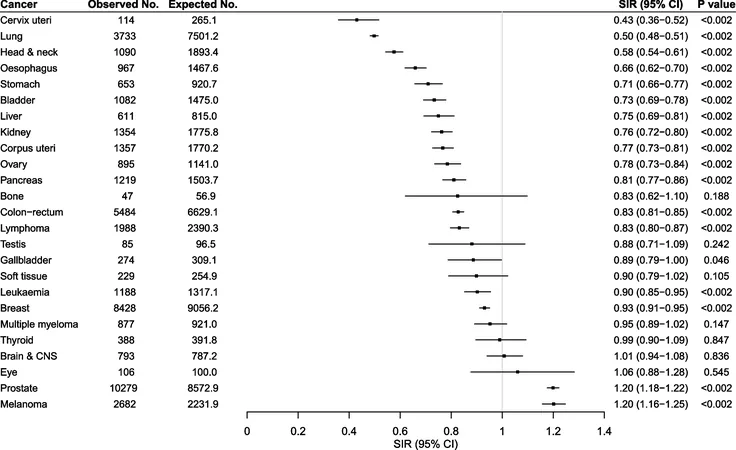
Did you know that India accounts for one in five cervical cancer cases globally? The majority of these cases stem from HPV, a virus that can lead to this deadly disease. While the vaccine has been available through private channels in India since 2008, uptake has been disappointingly low due to various factors including cost and misinformation stemming from adverse events in unrelated trials that have left the public wary.
Sutapa Biswas, co-founder of the Cancer Foundation of India, highlights a significant turning point: India has begun producing its own cervical cancer vaccine, which is expected to be incorporated into the national vaccination program by late 2023 or early 2024. Biswas expressed frustration over the years of potential lost due to misconceptions regarding vaccination costs: "So many times, we’d hear all kinds of excuses – ‘the cost is so high, we cannot vaccinate.’ But the cost of treating cancer is way higher."
The stakes are high. Each year, cervical cancer claims the lives of thousands of women in India – a tragic statistic that underscores the urgency of this initiative. To address this, last year, approximately 11,000 members of the Federation of Obstetric and Gynaecological Societies of India (Fogsi) undertook virtual training. Following this, about 100 trainees have ascended to the level of National HPV Faculty, set to educate an additional 500 general physicians from the Indian Medical Association over the next six months.
This comprehensive training covers everything from vaccine dosages to understanding the World Health Organization’s goals for cervical cancer elimination. It also prepares doctors to effectively answer common questions and address concerns within their communities.
Dr. Priya Ganeshkumar, a leading gynaecologist in the initiative, shared that many physicians did not realize that cervical cancer could be eliminated through vaccination. "The training helps them understand the importance of raising this topic with patients," she said, emphasizing that vaccination is not solely the responsibility of pediatricians. The ideal age for the HPV vaccine is pre-teens, making discussions with mothers vital when daughters visit for other health check-ups.
The COVID-19 pandemic has surprisingly aided this vaccination promotion effort, as awareness of vaccines has proliferated even in less-educated rural communities. "People now understand the connection between viruses and vaccines," says Biswas, fostering an environment conducive to discussing the HPV vaccine.
Funding from organizations such as Cancer Research UK, which is contributing about 25% of the project's budget, further bolsters this initiative. The hope is to pave the way for a future where almost no woman will develop cervical cancer, a disease that is, heartbreakingly, preventable.
As India steps up to meet this monumental challenge, the convergence of training, community engagement, and newly available vaccines holds the potential to transform public health and save countless lives. With every presentation made and every conversation sparked, the dream of a cervical cancer-free future inches closer to reality.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)