Innovative Management of Abnormal Uterine Bleeding in Stem Cell Transplant Patients
2024-12-18
Author: Nur
For patients grappling with hematologic malignancies and undergoing treatments like stem cell transplantation, blood transfusions often become a lifeline. While the risks associated with transfusions, such as iron overload and severe reactions, are acknowledged, the advantages they offer typically overshadow the negatives. Anemia—a common complication in these patients—not only heightens symptom burden but also disrupts quality of life, sometimes resulting in extended hospital stays.
A significant contributor to the increased reliance on transfusions among premenopausal patients is abnormal uterine bleeding (AUB), particularly prevalent in those undergoing allogeneic hematopoietic stem cell transplantation (HSCT) due to prolonged pancytopenia. Recognizing this challenge, a multidisciplinary team at one medical institution devised a proactive algorithm utilizing leuprolide, a gonadotropin-releasing hormone (GnRH) agonist, possibly combined with continuous oral contraceptive pills (OCPs). This approach is innovative in that it aims to prevent and manage AUB systematically. Leuprolide suppresses the production of estrogen and progesterone, effectively creating a temporary menopausal state which can significantly reduce menstruation's frequency and severity.
The goal of this study was clear: to determine whether the implementation of leuprolide, with or without OCPs, could lower the rates of red blood cell (RBC) and platelet transfusions in premenopausal patients with hematologic malignancies undergoing their first HSCT. Data was meticulously gathered regarding transfusion needs and venous thromboembolism (VTE) occurrences, focusing primarily on the total transfusions required within a 90-day post-transplant window.
It’s essential to monitor VTE risks in patients receiving hormonal therapies due to their known association with thrombosis. As women undergoing HSCT already face an elevated risk for such thrombotic events from factors like reduced mobility during hospitalization, diligent observation is key.
Among the study cohort of 214 premenopausal women who underwent HSCT between June 2016 and January 2022, AUB was identified in 58.4% of participants. Results revealed that patients receiving leuprolide—either alone or with OCPs—had significantly reduced requirements for platelet and RBC transfusions. Specifically, those on the treatment algorithm received platelet transfusions 1.2 times less often and RBC transfusions 1.1 times less frequently than those not receiving medication.
Surprisingly, VTE events noted in 8.9% of the patients showed no significant correlation with age or treatment groups, indicating that the utilization of leuprolide did not escalate VTE risk, thus reaffirming the treatment algorithm's efficacy.
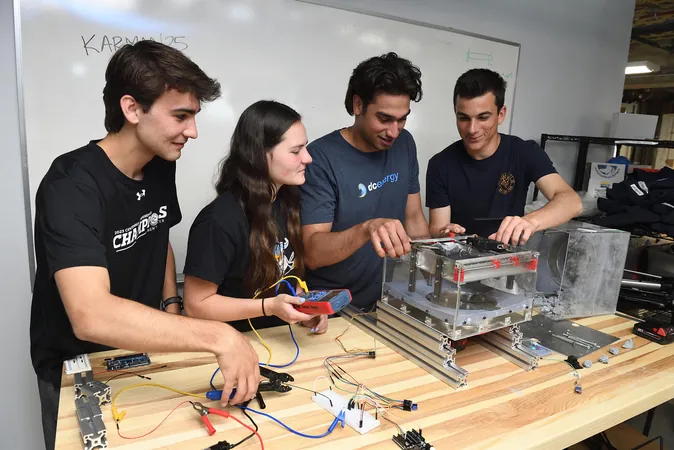
In light of these findings, oncology nurses play a crucial role in managing AUB among this patient demographic. Awareness of AUB as a common issue is imperative, as patients may not readily report changes in their menstrual patterns. To advocate effectively for preventative strategies, nurses should be proactive in assessing for AUB symptoms and educating patients about the benefits of using leuprolide and OCPs.
Additionally, it is recommended that leuprolide treatment commence at least one month prior to HSCT to forestall withdrawal bleeding during the conditioning phase.
In summary, addressing AUB in premenopausal women undergoing HSCT is vital for diminishing blood transfusion needs and enhancing patient outcomes. The application of leuprolide—either alone or alongside OCPs—demonstrates marked success in reducing transfusion requirements without amplifying VTE risk. Oncology nurses are pivotal in this coordinated effort, facilitating early identification and management of AUB while educating patients about treatment rationales. This integrative approach contributes significantly to better patient experiences during an already challenging therapeutic journey.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)