New Breakthrough Reveals How Hepatitis A Virus Exploits a Cellular Protein for Infection
2024-11-21
Author: John Tan
Introduction
Recent research has unveiled significant insights into how the hepatitis A virus (HAV) infiltrates and manipulates liver cells, potentially paving the way for innovative treatments against the highly contagious virus.
The hepatitis A virus, notorious for causing severe liver inflammation and widespread outbreaks, has impacted over 45,000 individuals in the United States since 2016, leading to hundreds of deaths, despite the availability of an effective vaccine since the 1990s.
Research Findings
Stanley M. Lemon, MD, a leading researcher at the University of North Carolina (UNC) School of Medicine, has dedicated decades to unraveling the complexities of HAV.
His latest findings reveal the pivotal role of a little-known protein, PDGFA-associated protein 1 (PDAP1), in the virus's ability to replicate and infect liver cells.
CRISPR Screening Results
Following an extensive CRISPR screening of over 19,000 human genes, Lemon and his team identified PDAP1 as a critical facilitator of hepatitis A infection.
This novel protein, previously lacking a defined function, was shown to be co-opted by the virus to aid in its replication processes within liver cells.
Role of PDAP1 in Cellular Stress Response
Delving into the function of PDAP1, the researchers discovered its importance in maintaining the cellular stress response, which becomes crucial when liver cells are under distress from infection or other stressors.
The liver, known for its resilience and recovery capabilities, can sometimes be pushed to the limits by pathogens like HAV, leading to severe health complications.
Experimentation and Results
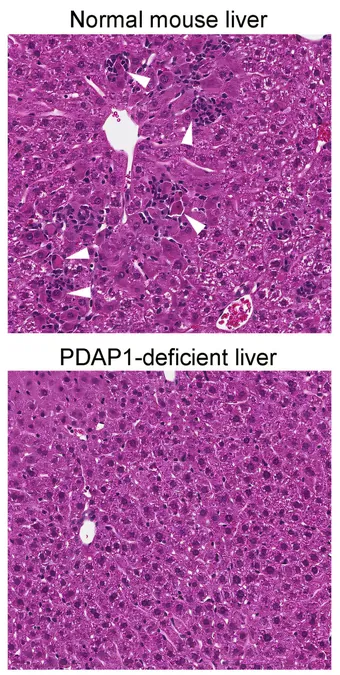
In their experiments, the team utilized CRISPR-Cas9 technology to "knock out" PDAP1 in cultured liver cells and in a mouse model.
The results were striking: Cells without PDAP1 failed to support HAV replication, and the genetically modified mice exhibited complete resistance to hepatitis A infection.
Implications for Broader Health Issues
Additionally, the researchers highlighted an intriguing linkage between PDAP1 and broader health issues, including cancer.
The integrated stress response—a mechanism that helps cells manage severe stress—was shown to be disrupted in the absence of PDAP1.
This disruption not only prevented the virus from reproducing but also hindered the cell's ability to cope with stress, suggesting that PDAP1's role extends beyond viral replication into cellular survival and function.
Future Directions
Dr. Lemon emphasizes the potential for expanded research into PDAP1, suggesting that insights into its cellular functions could unlock new knowledge about diseases ranging from viral infections to metabolic disorders and even cancer.
As scientists continue to probe the intricate relationship between viruses and host cellular mechanisms, the findings from UNC may herald new strategies for fighting infectious diseases and understanding cancer biology.
Conclusion
This research, published in Science Advances, invites further investigation into PDAP1 and the protections it offers to liver cells under threat.
The connection between viral infection, cellular stress responses, and cancer survival mechanisms may illuminate paths to innovative therapies that could benefit a wide array of health conditions.
Stay tuned as we delve deeper into how understanding hepatitis A could reshape our strategies in combating various diseases that exploit similar cellular processes!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)