New Study Unveils Alarming Connection Between Bacterial Infections and Liver Complications in Hepatitis B Patients!
2024-12-19
Author: Jia
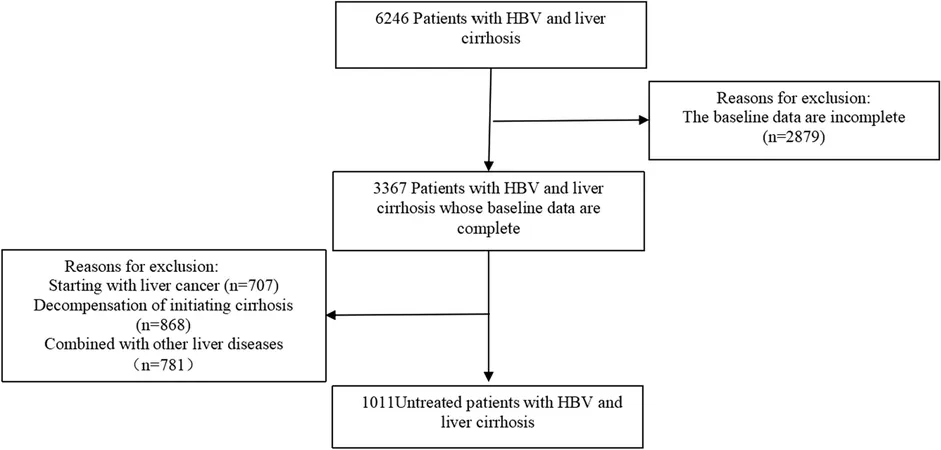
Recent research has shed light on a disturbing trend that threatens the health of patients with compensated cirrhosis related to the hepatitis B virus (HBV). Conducted at Tianjin Second People’s Hospital, this extensive retrospective study tracked 1,011 patients who began antiviral therapy from January 2013 to January 2024. The findings emphasize the considerable impact bacterial infections (BIs) have on the risk of hepatic decompensation, a severe complication often leading to critical health breakdowns.
Understanding the Study Population and Methods
The research commenced by carefully selecting patients based on strict inclusion and exclusion criteria to ensure the integrity of the data. Only individuals diagnosed with HBV-related compensated cirrhosis were considered, all of whom had never undergone antiviral therapy prior to this study. In contrast, patients suffering from co-infections, other severe liver conditions, or who had used certain medications were excluded.
The study assessed various clinical and laboratory parameters at the time of patients' first antiviral treatment, which provided a comprehensive overview of their health conditions. Among these parameters were liver function tests, bilirubin levels, and platelet counts, which play a crucial role in determining liver health and disease progression.
Key Findings: The UFO Effect of Bacterial Infections
Of the 1,011 participants, 89 patients (8.8%) experienced bacterial infections during their antiviral treatment. Alarmingly, among those who contracted infections, 40 (44.9%) progressed to hepatic decompensation, compared to only 9% of patients without infections. The study revealed that the risk of experiencing decompensation events significantly escalated when BIs occurred, with bacterial infections identified as formidable independent risk factors in patients with already fragile liver conditions.
Patients with BIs observed baffling statistics, with the mean time to decompensation being just under 44 months—indicative of a rapid health decline post-infection. The most common complication resulting from this was ascites, which developed in a considerable percentage of cases.
Types of Bacterial Infections: The Culprits Revealed
Digging deeper into the nature of these infections, the majority were categorized as pulmonary (50.5%), followed by urinary tract infections (17.8%). Escherichia coli was highlighted as a predominant pathogen, demonstrating a notable connection between specific bacterial strains and decompensating health outcomes in cirrhotic patients.
Additionally, the correlation between infection and the severity of liver damage was underscored by findings that revealed compromised patients often presented lower albumin levels alongside elevated liver stiffness and other abnormal liver function metrics.
The Bigger Picture: Implications for Healthcare and Patients
This pivotal study underlines a crucial message for healthcare professionals: addressing bacterial infections in hepatitic patients is not just a matter of treating an infection but is instrumental in averting the progression of liver disease. As BIs can lead to rapid deterioration of liver function, it is imperative for clinicians to meticulously monitor cirrhosis patients for any signs of infection during antiviral therapy.
Furthermore, with the rising prevalence of HBV-related liver disease globally, understanding these findings is critical in developing preventative strategies that could potentially mitigate the risks associated with BIs.
Concluding Thoughts: A Call to Action
This research is a clarion call for both medical communities and patients alike. For those suffering from HBV-related compensated cirrhosis, recognizing the signs of bacterial infections and seeking timely treatment can make all the difference. As our findings suggest, early intervention and stringent monitoring may not only prolong lives but also enhance the quality of life. Thus, let's get the word out and forge a proactive approach in managing health among vulnerable patient populations.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)