Nurses Revolutionize Post-ACS Care and Boost Patient Outcomes: The ALLEPRE Trial
2025-04-02
Author: Rajesh
In a groundbreaking revelation at the American College of Cardiology (ACC) 2025 Scientific Session in Chicago, a nurse-coordinated secondary prevention program has been shown to significantly decrease the risk of major adverse cardiovascular events (MACE) for patients recovering from acute coronary syndromes (ACS). The ALLEPRE trial, led by Dr. Giulia Magnani of the University of Parma, highlights the continued struggle against ACS, which remains a leading cause of morbidity and mortality worldwide.
Dr. Magnani emphasized that despite the availability of medical therapies and lifestyle interventions, real-world data consistently shows that secondary cardiovascular prevention strategies are underutilized. “Patients recovering from ACS struggle with the emotional and physical implications of their diagnosis, often resulting in subpar adherence to lifestyle changes and medication,” she pointed out.
Dr. Laura Davidson from Northwestern Medicine echoed these findings, stressing that ACS incidents can arise suddenly and force patients to make rapid and significant lifestyle adjustments. She remarked, “It’s overwhelming for patients; they need support not just from physicians, but from a dedicated healthcare team that includes nurses.
The ALLEPRE study assessed 2,057 patients admitted with various forms of ACS—specifically STEMI, NSTEMI, or unstable angina—across seven hospitals in Italy. Participants were randomly assigned to either a traditional care model, which included regular follow-ups with cardiologists, or a comprehensive nurse-led program that provided at least nine personalized educational sessions with nurse coordinators. These sessions focused on assessing cardiovascular risk profiles, ensuring medication adherence, promoting healthy lifestyle choices, and offering referrals for additional support as needed.
The trial involved 250 specialized cardiology nurses, who underwent rigorous centralized training in cardiovascular prevention, benefiting from an interdisciplinary approach that included insights from medical, nursing, and psychological domains. This well-organized structure is marked as a pivotal moment in patient care within the realm of cardiovascular health.
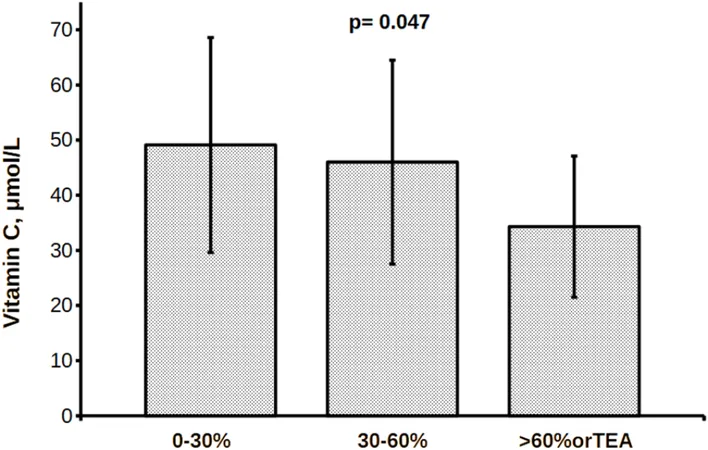
Key findings from the study revealed that patients engaged in the nurse-led care experienced a reduction in the combined rates of cardiovascular death, nonfatal heart attacks, and nonfatal strokes over a seven-year period, compared to those under standard care. Interestingly, while medication adherence improved in both groups, traditional metrics such as LDL cholesterol and blood pressure did not show significant improvements, leading researchers to ponder the mechanisms behind the trial’s successes.
Dr. Vera Bittner from UAB Medicine commended the nurse-led program, noting, “It’s exciting to see an intervention that truly changes patient outcomes.” The focus appeared to be on behavior modification—nurses played an essential role in guiding patients through necessary lifestyle changes by fostering an environment of trust and support.
Magnani concluded, “The early benefits of this structured program suggest that not only can we empower patients but we can also bolster our healthcare system's approach to secondary prevention.” With plans for future research and a cost-effectiveness analysis underway, the findings indicate a potential paradigm shift in how we approach post-ACS patient care.
In reflecting on these promising results, healthcare professionals are encouraged to reconsider the role of nurses in cardiovascular prevention—a change that could not only improve patient lifestyles but ultimately save lives. This pivotal moment is clear: empowering nurses can lead to revolutionary improvements in post-ACS care.
Stay tuned for further updates as the medical community seeks to implement these findings on a broader scale.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)