Post-TAVI Pacemaker Linked to Dismal Long-Term Outcomes: A Wake-Up Call for Patients and Physicians!
2025-04-08
Author: Jia
Unveiling the Long-Term Risks
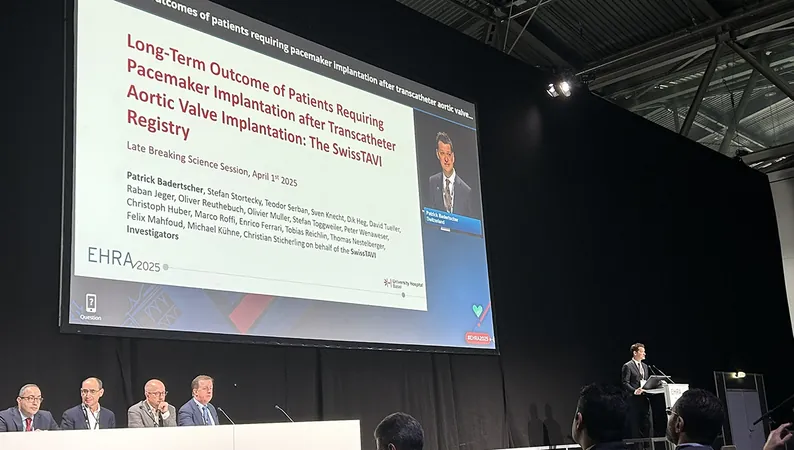
In a groundbreaking analysis of the Swiss TAVI registry, researchers have uncovered alarming evidence that patients needing a pacemaker within 30 days following Transcatheter Aortic Valve Implantation (TAVI) face a significantly heightened risk of mortality, both from all causes and cardiovascular issues, stretching out as far as a decade later.
The study highlights a concerning trend: patients who received a new pacemaker after their TAVI procedure experienced a measurable decline in Left Ventricular Ejection Fraction (LVEF) and had an increased prevalence of severe heart failure symptoms during follow-ups compared to those who did not require pacing.
Dr. Patrick Badertscher from the University Hospital Basel stressed the importance of exploring novel pacemaker implantation techniques, such as conduction system pacing, which may lead to varied outcomes in TAVI patients. However, he noted that clear evidence of superiority in outcomes for these new techniques within this specific patient population is not yet available.
As TAVI procedures become more prevalent among younger, lower-risk patients, the implications of these findings become crucial. Dr. Amit Vora from Yale School of Medicine pointed out that while significant advancements have been made to decrease the need for permanent pacemakers over the last five years, the observed long-term mortality risks raise critical questions for both patients and healthcare providers alike.
Experts Weigh In on Solutions
The study analyzed data from 13,360 patients (average age of 82; 47% females) who underwent TAVI between February 2011 and June 2022. Among these individuals, 10% already had a pacemaker at the time of the procedure, while 15% required a new one post-TAVI. Notably, patients who received a new pacemaker were generally older, had a greater likelihood of being male, and had higher instances of comorbidities such as atrial fibrillation, diabetes, and hypertension.
Follow-up assessments revealed that those implanted with a new pacemaker had a 15% increased risk of all-cause mortality and a 25% increased risk of cardiovascular death after one year, compared to their pacemaker-free counterparts. Furthermore, these patients were found to experience notable declines in heart function and worse symptoms of heart failure.
These mortality risks showed little improvement even after five and ten years, indicating a substantial long-term burden tied to the need for a pacemaker following TAVI.
While acknowledging the limitations of the study, including potential residual confounding factors and the absence of data regarding pacing burden over time, Dr. Vora emphasized the need for ongoing innovations in procedural techniques. He explained that techniques focused on ensuring a shallower depth of valve implantation could potentially minimize the need for pacemakers, although this may complicate future interventions.
Dr. Vora also cautioned that ongoing assessment of left ventricular function and pacing burdens in patients requiring permanent pacemakers post-TAVI is vital since chronic right ventricular pacing may have deleterious effects.
Given the gravity of these findings, both physicians and patients must remain vigilant and proactive in understanding the implications of pacemaker needs after TAVI procedures. With advancements in medical techniques constantly evolving, the focus should remain on individualized care strategies that enhance patient outcomes while mitigating risks associated with technological interventions.
As this research shines a spotlight on the potential consequences following TAVI, it serves as a crucial reminder for healthcare providers to carefully evaluate and refine their procedures, striving towards better, safer cardiac care for patients everywhere.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)