Revolutionary AI Breakthrough Unveils Four Distinct Long COVID Patient Subgroups!
2025-01-10
Author: Daniel
A groundbreaking study spearheaded by researchers at the esteemed Perelman School of Medicine, University of Pennsylvania, is set to transform long COVID care across the United States! This research harnesses the power of artificial intelligence (AI) to accurately categorize long COVID patients into four distinct subgroups, recognizing the diverse needs among patients and improving treatment strategies in hospitals.
As hospitals vary widely in terms of equipment, staffing, and patient demographics, tailoring care to meet the specific needs of local populations is more than just a necessity; it's now a promise made possible by AI. The newly published findings in the journal Cell Patterns reveal an innovative application of technology that leverages electronic health records to pinpoint what specific care services are required for long COVID patients at different healthcare facilities.
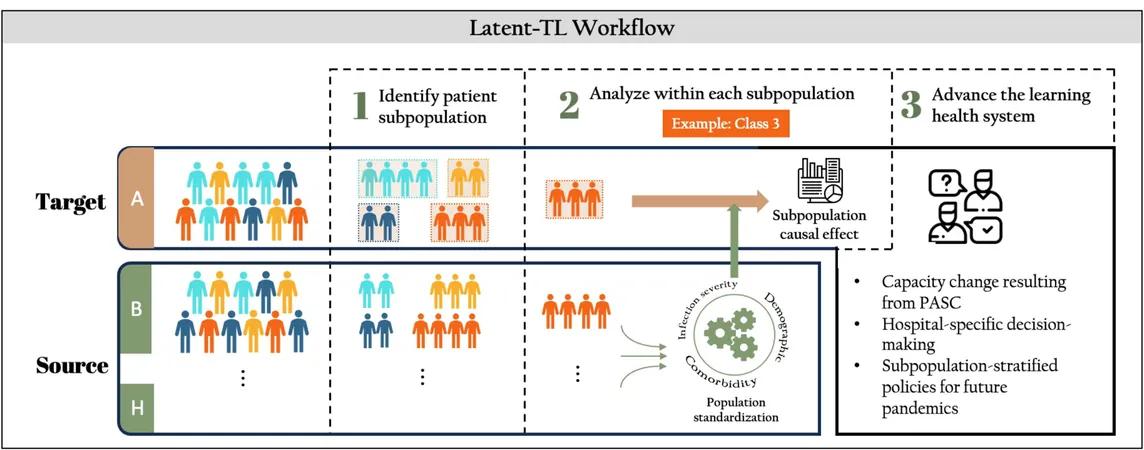
The AI system utilized a machine learning technique known as "latent transfer learning," which analyzed de-identified data from patients across eight pediatric hospitals. This analysis resulted in the identification of four significant patient subpopulations, each with unique characteristics:
1. Mental health conditions
This subset includes individuals suffering from anxiety, depression, neurodevelopmental disorders, and ADHD.
2. Atopic/allergic chronic conditions
Patients with asthma or severe allergies fall into this category, often requiring specialized treatment approaches.
3. Non-complex chronic conditions
This group comprises those with relatively straightforward health issues like vision problems or insomnia.
4. Complex chronic conditions
The most vulnerable patients in this subgroup suffer from heart or neuromuscular disorders, necessitating intricate care strategies.
The implications of these findings are monumental. By identifying these specific subpopulations, clinicians can move away from the ineffective "one-size-fits-all" model of treatment. Dr. Qiong Wu, who led the study, emphasized that high-risk subgroups often require tailored care — their analysis indicated that patients with complex chronic conditions see the highest rates of emergency visits and hospitalizations.
Moreover, the AI system outlines where resources need to be allocated within hospitals, providing actionable insights that can enhance patient care. Dr. Wu posited that if this machine learning framework had been deployed during the early days of the COVID-19 pandemic, it could have significantly improved hospitals' ability to prepare for surges in specific patient needs, such as ICU capacities and ventilator availability.
As we look beyond the COVID-19 crisis, the potential applications of this AI technology are vast. Chronic illnesses like diabetes, heart disease, and asthma vary tremendously across different regions, affected by factors such as healthcare resources and demographic profiles. The ability to customize treatment plans and resource allocation based on real-time data can redefine how hospitals manage both common and complex conditions.
The researchers are optimistic that this AI system can be adopted across numerous healthcare settings with a straightforward data-sharing infrastructure. Even hospitals not yet utilizing machine learning can gain immensely from shared information, ensuring no patient is left behind.
Could this revolutionary study mark the dawn of a new era in personalized healthcare? The future of patient treatment and resource management could very well depend on these insightful findings!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)