Revolutionary Blood Clots on a Chip Technology Paves the Way for Advanced Thromboinflammation Treatments!
2025-04-03
Author: Jia
Groundbreaking Development from Emory University
In a groundbreaking development from Emory University, researchers have unraveled a new model that could dramatically enhance our understanding and treatment of blood clots—conditions linked to life-threatening emergencies such as sepsis, heart attacks, strokes, and sickle cell disease.
Introduction of Thromboinflammation-on-a-Chip Model
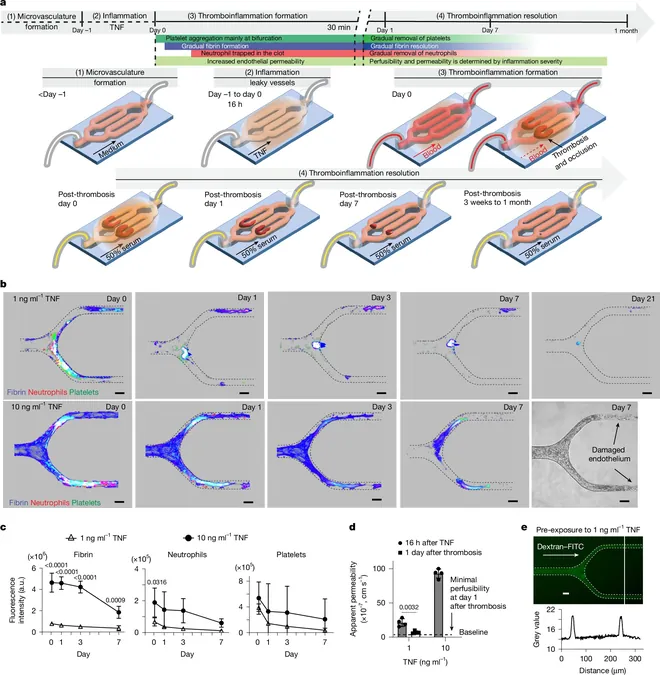
Published in the prestigious journal *Nature*, this innovative research introduces a “thromboinflammation-on-a-chip" model—an advanced system that replicates the human vascular environment, allowing for prolonged observation of blood clots over several months. Unlike existing models that can only maintain clots for short periods, this new approach uses 3D microvessels to create a more accurate and human-like simulation.
Expert Insights on Clot Resolution
Wilbur Lam, one of the study’s leading authors and a professor at Emory University, emphasizes the crucial need for advancements in this area: “Little is known about how blood clots resolve after an individual survives major cardiovascular events. Our chip technology allows us to observe and understand the entire resolution process of a clot, which has never been accomplished before.”
Functionalities of the Chip
The chip enables researchers to not only track clots but also evaluate various treatment strategies effectively. This model integrates essential human cells that participate in the clot resolution process, offering insights that other laboratory models simply could not provide. “The chip allows us to monitor changes in real time and under conditions that closely mimic those found in actual patients,” explains Yongzhi Qiu, another co-author of the study.
Broader Clinical Implications
As the implications of this research extend beyond stroke and cardiac arrest, it’s essential to note that other medical conditions like hypertension, diabetes, and severe trauma contribute to thromboinflammation, affecting a significant portion of the population. This new model stands to revolutionize the current paradigms in thromboinflammatory research.
Key Findings on Neutrophils and tPA
Further analyzing their findings, the researchers discovered that neutrophils—a type of white blood cell—play a crucial dual role in both resolving thrombi and triggering inflammation. Additionally, they shed light on the action of tPA or Tissue Plasminogen Activator, a treatment administered after strokes that not only aids in blood clot breakdown but also repairs damaged blood vessels, a previously unknown benefit.
Potential for Future Treatments
Moreover, the potential therapeutic implications extend to patients undergoing bone marrow transplants. The research suggests that certain drug combinations could alleviate veno-occlusive disease, a challenging complication characterized by blocked blood flow in the liver due to high doses of chemotherapy.
Significance for Clinical Trials
“Mapping blood clot behavior under inflammatory conditions allows us to hypothesize which treatments will be most effective and under what circumstances,” adds Lam, highlighting the study’s significance in paving the way for future clinical trials aimed at saving lives.
Future Directions in Thromboinflammation Treatment
As researchers continue to explore this innovative model, the future of thromboinflammation treatment looks promising, with the potential to customize medication timing and dosages like never before. The fight against the dangers of blood clots may just be entering a new era, one where lives can be saved with precision and understanding of human biology. Keep your eyes peeled for more on this developing story!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)