Revolutionary Coating Slashes Bone-Implant Integration Time by 50%!
2024-12-13
Author: Arjun
Introduction
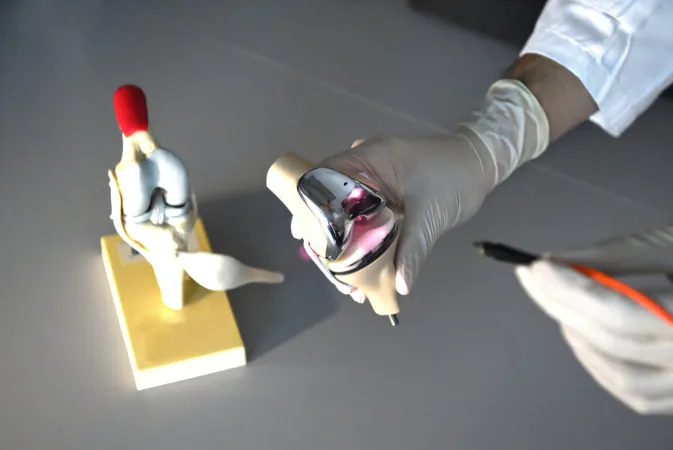
In an exciting breakthrough, a dedicated research team has unveiled a ground-breaking photocurrent-responsive coating for orthopedic implants that cuts the bone-to-implant integration time down to just two weeks! This innovative development not only speeds up recovery for patients but also significantly reduces the risk of implant rejection, a common concern in postoperative care.
Research Leadership and Focus
Under the leadership of Professor Kelvin Yeung Wai-kwok from the Department of Orthopedics and Traumatology at the University of Hong Kong (HKUMed), the team is now looking into the application of this cutting-edge technology in artificial joint replacements, aiming to transform procedures like knee replacements prevalent in Hong Kong.
Challenges with Osteoimmune Integration
Post-operative complications can arise when the osteoimmune microenvironment becomes unstable, which could impede the integration of implants and prolong recovery times. The revolutionary team has addressed this challenge with a specially designed near-infrared (NIR) light-responsive surface that enhances the body’s natural healing processes. This coating effectively modulates the macrophage response, dramatically lowering acute inflammation during the pivotal initial healing phase.
Mechanism of Action
By generating a photocurrent in response to NIR light, the innovative coating enhances calcium influx in macrophages—key immune cells that initiate the inflammatory response. This favorable shift in the osteoimmune environment encourages the recruitment of mesenchymal stem cells (MSCs), essential for bone formation, thus speeding up the integration process significantly.
Research Findings
The research, published in the prestigious journal Advanced Functional Materials, reveals just how transformative this technology can be. When tested on a tibial defect animal model, the integration period was reduced from a typical 28 days to an astonishing 14 days—effectively doubling the speed of recovery.
Implications for Orthopedic Surgery
But what does this mean for the future of orthopedic surgery? Many implants, especially those made of titanium dioxide (TiO2), face challenges in terms of responsiveness to NIR light. By employing hydroxyapatite (HA)—the primary mineral component found in bones—as the base for this new coating, the research team has unlocked a unique ability to create reactive surfaces that adapt to the body's biological responses.
Expert Insights
“We have created a surface that dynamically modulates the macrophage response in line with the patient’s healing timeline,” Professor Yeung explains. “This method significantly hastens bone-to-implant integration, doubling the success rate of fusion.”
Future Perspectives
As the field of orthopedic surgery continues to evolve, this revolutionary discovery not only promises to improve patient recovery times but also provides a fresh perspective on managing immune responses and minimizing the risks associated with implant procedures.
Conclusion
Could this groundbreaking technology become the standard in hospital operating rooms? With the potential to enhance success rates in orthopedic surgeries and minimize complications linked to implant failures—a staggering 10% of which are associated with loosening—this research lays the groundwork for future innovation in orthopedic biomaterials and techniques.
Next Steps
Stay tuned as we follow the developments in this groundbreaking research that could change the landscape of orthopedic surgery for years to come!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)