Revolutionary Discovery: Targeting Asxl1 Gene Boosts Immunotherapy Success in Cancer Treatment!
2024-10-11
Author: John Tan
Revolutionary Discovery: Targeting Asxl1 Gene Boosts Immunotherapy Success in Cancer Treatment!
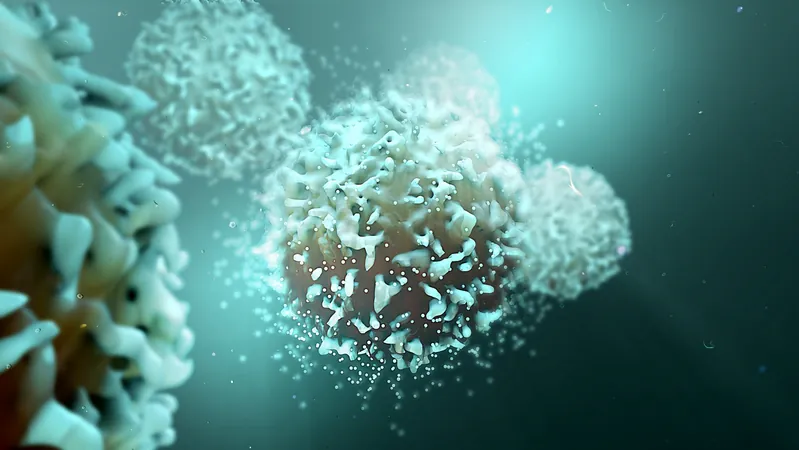
In a groundbreaking study, researchers from St. Jude Children's Research Hospital, in collaboration with other esteemed institutions, have unveiled how disrupting the Asxl1 gene in T cells can significantly enhance patients' responses to immune checkpoint blockade (ICB) therapy. These exciting findings, published in the prestigious journal Science, promise a transformative approach to cancer treatment, potentially increasing long-term tumor control for many patients undergoing ICB therapy.
ICB therapies have made remarkable strides in treating various cancers—including melanoma, lung cancer, and bladder cancer—leading to improved survival rates of between 20-40%, as reported by the American Cancer Society. However, a significant hurdle remains: the majority of patients continue to show minimal response to these therapies, leaving them in dire need of novel treatment strategies.
Driven by a quest to understand the intricacies of immune responses to ICB therapy, the research team investigated why certain patients exhibit positive outcomes while others do not. A particular focus was placed on the exhaustion of CD8 T cells, which often fails to mount an effective fight against tumors after prolonged exposure to immunotherapies.
In their meticulous research, the team examined a select group of patients diagnosed with myelodysplastic syndrome (MDS) who experienced remarkable long-term survival after receiving anti-PD-L1 treatments. They discovered that the Asxl1 gene was mutated in the T cells of all these patients, prompting further exploration into its role.
By knocking out the Asxl1 gene in mouse models, the scientists revealed that these altered T cells led to superior tumor control during checkpoint blockade, and the impact was significantly more sustainable compared to mice retaining the Asxl1 gene. This discovery pointed to the epigenetic functions of Asxl1—specifically, its regulatory role within the polycomb group-repressive deubiquitinase (PR-DUB) complex, which is pivotal in sustaining T cell function and hindering their exhaustion.
"This research highlights Asxl1 as a crucial epigenetic checkpoint that governs the pivotal transition of T cells into an exhausted state," explained co-corresponding author Dr. Ben Youngblood. "By navigating past this checkpoint, we can engineer T cells for a more durable and effective anti-tumor response.”
These findings open new avenues for improving immunotherapy, suggesting that editing the Asxl1 gene in T cells could yield long-lasting effects in cancer treatments. While this research is just the tip of the iceberg, it lays the groundwork for future innovations in immunotherapy and potentially saves countless lives.
As Dr. Peter A. Jones of the Van Andel Institute aptly put it, "Today's findings demonstrate how epigenetics can further enhance these powerful treatments to help even more individuals affected by cancer. This is an exciting time for cancer therapeutics!”
This major advancement in understanding the genetic underpinnings of immunotherapy could change the landscape of cancer treatment as we know it, possibly leading to more effective strategies that bring hope to patients who have been running out of options. Stay tuned, as this study promises to catalyze a wave of future research aimed at decoding the mysteries of cancer and immunotherapy!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)