Revolutionary Microwave Ablation Technique Demonstrates Precision and Safety for Prostate Cancer Patients!
2024-11-21
Author: Rajesh
Overview of the VIOLETTE Trial
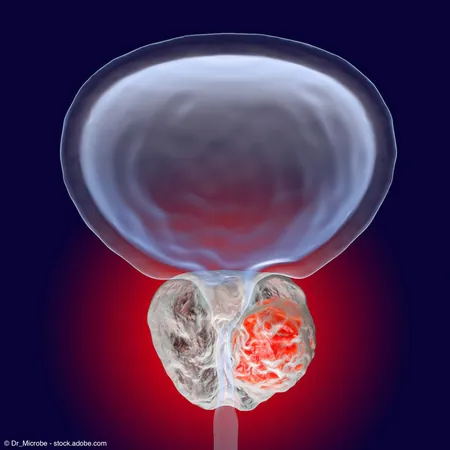
Recent findings from the phase 2 VIOLETTE trial (NCT04582656) indicate that targeted microwave ablation (TMA), enhanced by organ-based tracking (OBT) fusion technology, is proving to be a precise and safe treatment option for patients suffering from intermediate-risk prostate cancer.
Study Results and Participant Data
The results, published in the BJUI Compass, marked the completion of the study’s enrollment, with 76 carefully selected patients demonstrating a single focus of prostate cancer visible on MRI. Lead investigator Dr. Nicolas Barry-Delongchamps expressed enthusiasm, stating, 'The Koelis technology not only facilitated the detection and detailed characterization of these tumors but also allowed for meticulous planning of targeted treatments. As we await the final oncologic outcomes, we have strong confidence in this image-guided, needle-based technique as a promising option for carefully chosen patients.'
So far, the trial has enrolled 37 patients from five clinical trial sites across France and Belgium, with a median age of 68 years. Participants underwent TMA procedures either under general anesthesia or conscious IV sedation within an outpatient setting, with an average anesthesia duration of 78 minutes. Notably, a significant majority (70%) of procedures were completed transperineally, showcasing the method’s adaptability.
Adverse Events and Patient Outcomes
All participants received a median of three (ranging from 2 to 4) 12-watt ablations, lasting between 2 to 5 minutes each, followed by a median follow-up period of six months. Despite the introduction of a novel treatment method, the trial recorded 58 adverse events across 22 patients, primarily mild (74% grade 1), with only a few classified as severe.
Crucially, the investigators reported no substantial changes in key metrics such as the International Prostate Symptom Score or sexual health questionnaires from the initial baseline to the follow-up period, indicating that the quality of life for patients remained stable following treatment.
Imaging and PSA Density Results
One of the standout achievements of the study was reflected in post-procedure imaging; 36 out of 37 evaluable patients (97%) showed visible non-vascularized prostatic tissue on DCE MRI just seven days post-treatment. This non-vascularized area exceeded the targeted tumor index by over 100%, with a median volume of 6 mL.
Moreover, there was a noteworthy decrease in the prostate-specific antigen (PSA) density, dropping from 0.2 ng/mL at the start to 0.1 ng/mL by the 12-month follow-up. This could potentially signal promising treatment outcomes.
Future Directions and Study Goals
Koelis, the driving force behind the technology, confirmed the enrollment of the final subject for the trial in September 2024. With the VIOLETTE trial still ongoing, further follow-up and data collection will be essential to corroborate these initial findings.
The primary focus of the VIOLETTE study is to evaluate treatment efficacy, specifically the absence of ISUP grade 2 or higher cancer on targeted biopsy at one year. Additional objectives involve assessing safety parameters, urinary and sexual outcomes, PSA kinetics, alongside MRI treatment zone shape at specified follow-up periods.
Conclusion and Implications
As researchers continue to monitor outcomes, the implications of this cutting-edge ablation technique could revolutionize prostate cancer treatment, offering new hope to those battling this common adversary. Stay tuned as we uncover more insights from this groundbreaking study!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)