Revolutionary Tiny Vesicles Offer Hope to Diabetic Patients Facing Amputation
2024-11-25
Author: Arjun
Title: Revolutionary Tiny Vesicles Offer Hope to Diabetic Patients Facing Amputation
In a groundbreaking study, scientists are on the verge of unveiling a potential game-changing treatment for diabetic limb ischemia, a severe complication linked to diabetes that significantly raises the risk of limb amputation. This condition is characterized by diminished blood flow to the legs and feet, resulting in chronic pain, persistent ulcers, and, in the most severe circumstances, amputation — making it the leading cause of non-traumatic limb loss.
Patients afflicted with diabetic limb ischemia face grim statistics: they have a 20% to 30% higher chance of experiencing cardiovascular events and an astonishing 14 times greater risk of amputation compared to individuals with other arterial diseases.
“Our key aim is to identify a safer, non-surgical alternative for patients suffering from restricted blood flow and tissue damage in their limbs,” stated Xing Zhang, a researcher from the Department of Vascular Surgery at Shanghai Ninth People's Hospital, and one of the authors of a study recently published in Advanced Healthcare Materials. Current treatment options are often invasive, involving surgery or medications that carry risks and do not always yield successful outcomes.
After a decade of exploring stem cell therapies for vascular ailments, Zhang and his team faced significant hurdles such as immune rejection, tumor development, ethical issues, and unstable survival rates of the cells. They needed to pivot to a more viable solution: extracellular vesicles.
The Promise of Extracellular Vesicles
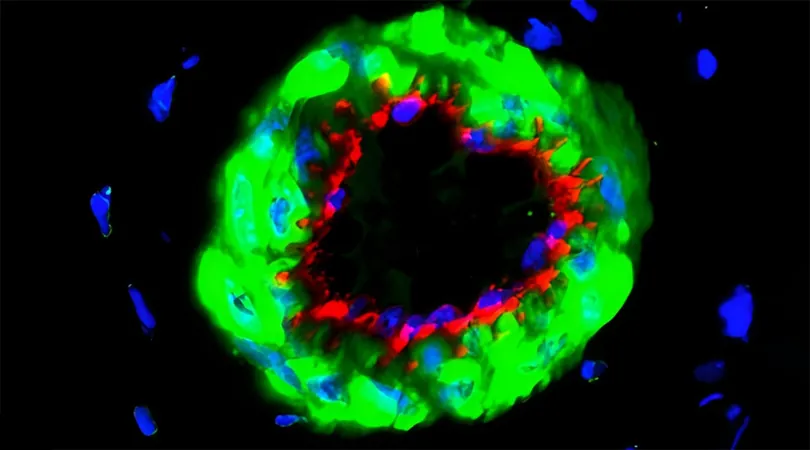
Extracellular vesicles are tiny, lipid-bound particles that naturally disperse from nearly all cell types, carrying crucial biomolecules. According to the research team, “Transplantation of extracellular vesicles, particularly exosomes, has notable advantages over traditional stem cell therapies,” bypassing many obstacles faced by previous treatments.
A crucial aspect of this new therapy is identifying proteins or genes that can guide these vesicles to improve their efficacy in targeting the disease. By adjusting specific proteins to align with particular receptors or pathways, researchers can ensure that vesicles deliver therapeutic molecules exactly where they are needed, thereby enhancing treatment effectiveness while reducing side effects.
Investigating Netrin1
Previous research highlighted the protein Netrin1, known for its protective function within the cardiovascular system, as it helps encourage blood vessel growth, cell survival, and decreases inflammation. “Though primarily recognized for its role in nerve development, Netrin1 could also hold significant therapeutic potential for diabetic limb ischemia,” explained Xinwu Lu, Director of Vascular Surgery at Shanghai Ninth People's Hospital.
Despite the promising prospects, the role of Netrin1 in diabetic limb ischemia was largely unexplored, prompting the team to examine its levels in blood and tissue samples from patients suffering from the condition compared to those with acute arterial embolism.
Their findings were compelling: Netrin1 levels were markedly lower in patients with diabetic limb ischemia, suggesting that reduced levels of this protein may be implicated in the disease’s progression. This discovery spurred further investigation into Netrin1 as both a disease marker and a possible therapeutic target.
A New Healing Approach
The researchers aimed to utilize genetically modified stem cells, derived from adipose (fat) tissue, to enhance Netrin1 production. These cells would release exosomes loaded with Netrin1 as a part of their normal functions. Through a specialized purification method called differential ultracentrifugation, the team isolated exosomes, ensuring they carried higher concentrations of Netrin1 before injecting them directly into ischemic tissues.
Initial experiments demonstrated that Netrin1-enriched exosomes outperformed standard exosomes from adipose-derived stem cells. “Netrin1 activates protective cell pathways, allowing them to better withstand stress,” noted Yihong Jiang, a postdoctoral researcher involved in the study. The exosomes not only promote blood vessels' growth but also significantly enhance the healing capacity of the affected tissues.
By targeting two critical pathways associated with cell survival and repair, Netrin1-enriched exosomes provide a ‘protective shield’ that accelerates recovery for cells in compromised blood vessels, offering a promising alternative to traditional invasive methods.
Towards Clinical Application
Though the prospect appears bright, there remain challenges ahead for the application of this innovative therapy. “We need to develop a reliable delivery system to maintain the stability and efficiency of the exosomes in the body,” Xinwu cautioned. Producing consistent high-quality exosomes is also paramount for ensuring safety and efficacy in clinical settings.
Moreover, monitoring Netrin1 levels in the blood could help healthcare providers identify high-risk diabetic patients early on, allowing for proactive intervention and potentially thwarting disease progression. While Netrin1 may show promise as a diagnostic tool, ongoing research is required for clinical validation.
The next steps for the research team involve conducting larger animal studies to further explore the effects and safety of Netrin1-enriched exosomes, with hopes of initiating preliminary human trials soon. “Our ultimate objective is to pioneer this transformative therapy into clinical practice, offering diabetic limb ischemia patients a safe, non-invasive treatment option,” Zhang concluded.
This innovative approach represents not only a major leap in the treatment of diabetic complications but also instills hope for millions struggling with the potentially devastating consequences of diabetes. Stay tuned, as the future of diabetic care may be just around the corner!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)