Shocking Case of Adult Acute Necrotizing Encephalopathy Linked to Bacterial Infection!
2024-10-07
Author: Daniel
In a perplexing medical case, a 46-year-old woman found herself battling for her life against an aggressive form of Acute Necrotizing Encephalopathy (ANE) triggered by a bacterial infection. This shocking incident serves as a stark reminder of the dangers lurking behind seemingly ordinary infections, especially in adults, a demographic rarely associated with this condition.
Upon her admission to the hospital, the woman was in dire straits—intubated with a Glasgow Coma Scale score of only 3 out of 15. Her harrowing symptoms included a staggering fever of 41 °C, chills, nausea, vomiting, and a serious impediment to consciousness. Strikingly, she displayed no signs of typical respiratory distress like cough or hemoptysis, which often accompany such severe illnesses.
Having a medical history primarily marked by kidney stones and intermittent lower back pain, there were no signs of prior neurological episodes or toxic exposures. Blood tests revealed a distressing array of abnormalities: high levels of inflammation markers including procalcitonin, CRP, and interleukin-6, along with severely elevated liver enzymes hinting at underlying organ distress.
Amidst this chaos, a potential E. coli infection was uncovered from initial blood cultures. However, this revelation took a backseat as follow-up cultures indicated a different picture, embroiled in confusion due to the use of potent antibiotics before testing.
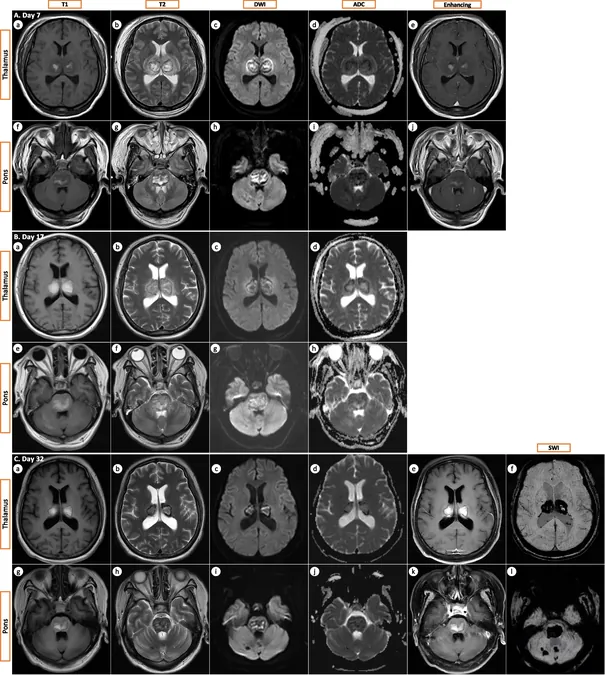
Testing for various viral pathogens turned out negative, while comprehensive investigations, including lumbar puncture and advanced MRI imaging, indicated typical ANE lesions in the brain, raising the alarm for immediate intervention. Her MRI scans revealed ominous hyperintense lesions affecting critical regions such as the thalami and pons, characteristic of ANE.
In a desperate bid for survival, the medical team embarked on aggressive treatment, including broad-spectrum antibiotics and immunotherapy with methylprednisolone. Remarkably, after relentless effort spanning over three weeks in intensive care, she was eventually discharged in a minimally conscious state but managing to respond to painful stimuli.
The case is groundbreaking, marking one of the rare instances of adult-onset ANE linked to bacterial infections rather than the more commonly seen viral triggers such as COVID-19 or influenza. The findings stress the need for awareness that bacterial infections could also inflict such devastating outcomes, potentially influencing future diagnostic and treatment protocols.
Further examination revealed the patient to have residual disabilities, yet a follow-up appointment nine months post-admission demonstrated significant communication abilities, although she faced ongoing challenges with her legs. This puzzling evolution of symptoms and the patient’s gradual improvement raises crucial questions about the pathogenesis of ANE.
Experts theorize that rather than being a direct effect of a pathogen attacking the brain, ANE is likely a result of a severe immune response—a cytokine storm—impacting the brain's microvasculature. This inflammatory response leads to axonal injury and cell death, underscoring the potential for sepsis from bacterial infections to contribute lucratively to ANE onset.
Current research highlights the urgent need for more case studies to differentiate between bacterial and viral causes of ANE and their respective prognoses. The implications of this case could shift medical understanding, leading to earlier interventions and potentially better outcomes for patients across various demographics.
In conclusion, this extraordinary case not only broadens the landscape of ANE's causative factors but also emphasizes the critical nature of timely and accurate diagnosis. As we delve deeper into understanding this enigmatic condition, every finding could pave the way for groundbreaking advances in treatment methodologies and patient care strategies.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)