Shocking Discovery: How Liver Cancer Stem Cells Manipulate the Immune System to Fuel Disease Comebacks!
2024-10-09
Author: Nur
Introduction
Recent research spearheaded by Stanford Medicine has unveiled alarming new insights into liver cancer recurrence, revealing that certain cancer cells are capable of enlisting immune cells as protective shields. This clever strategy allows the cancer to resist treatment, leading to distressing relapses.
Targeting Macrophages
In their groundbreaking study, researchers targeted a subset of immune cells known as macrophages. They discovered that liver cancer cells cozy up to these macrophages, which not only fail to launch an attack but actually aid in fostering an environment conducive to tumor survival and proliferation. The team demonstrated that two drugs that disrupt this relationship effectively eliminated cancer cells in mouse models of recurrent liver cancer and significantly impeded tumor recurrences.
Mapping Residual Cancer Cells
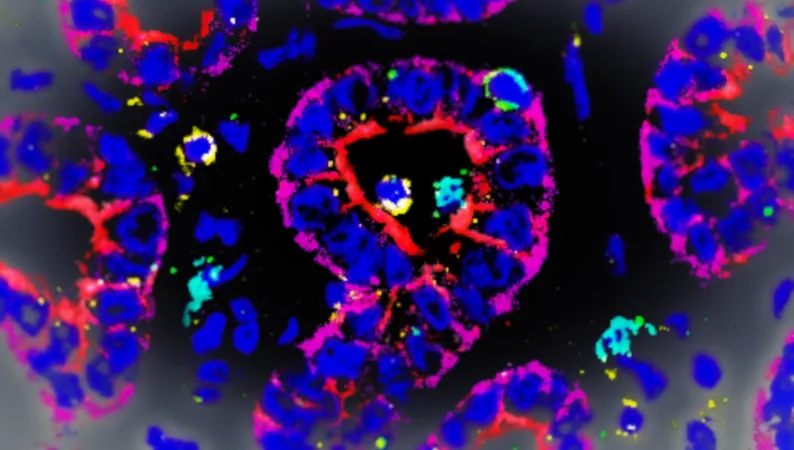
Using advanced techniques crafted at Stanford Medicine, the researchers meticulously mapped over one million single cells across more than 100 human liver tumor samples following chemotherapy. While this treatment, particularly chemoembolization, is often initially successful, it frequently leads to tumor resurgence within months. This begs the question: Where do these elusive residual cancer cells hide?
“Our goal was to pinpoint the elusive locations where these residual tumor cells are lurking,” said Renumathy Dhanasekaran, MD, assistant professor of gastroenterology and hepatology. “The biological ZIP code of these cells is critical, as they form a protective bubble around themselves with macrophages. This camouflage prevents detection and attack by other immune cells, thus allowing them to hibernate before initiating another wave of tumor growth.”
Challenges in Research
Remarkably, this survival tactic permits these tumor cells to function like cancer stem cells, lying dormant and undetectable for weeks or even months.
The researchers faced numerous hurdles to illuminate this process. Analyzing residual disease in solid tumors like liver cancer is inherently challenging due to treatment-induced cellular death creating skewed samples. However, advancements in computational techniques and machine learning proved essential in making sense of the complex tumor microenvironment, where the interactions of different cell types were mapped with precision.
Findings from Biopsies
Through comprehensive biopsies of 108 previously treated liver tumors, researchers employed a spatial mapping method known as co-detection by indexing (CODEX), unveiling a trove of information regarding the cell types within these tumors. They found significant differences between treated and untreated tumors, discovering that treated tumors had a higher prevalence of immune-suppressing cancer cells and macrophages, specifically those classified as M2-like macrophages. These specific macrophages were found to cocoon the cancer cells, reducing immune system effectiveness.
Molecular Interactions
Further investigation revealed a molecular dialogue between these stem-like cancer cells and M2-like macrophages, centered around two key cancer-associated molecules: TGF beta and PDL1. The presence of PDL1 inhibits T cell activity while TGF beta can actually promote tumor growth by reducing immune responses.
“We theorize that the macrophages expressing PDL1 bolster tumor growth by activating TGF beta and inducing T cell fatigue,” stated Dhanasekaran.
Potential Therapeutic Strategies
Encouragingly, results from mouse models showed that inhibiting both PDL1 and TGF beta enhanced the immune response against cancer and eliminated residual cells, greatly reducing the likelihood of recurrence.
In light of these findings, Dhanasekaran expressed optimism about future implications, emphasizing that drugs targeting PDL1 and TGF beta have already undergone human trials for other diseases. “By eradicating these tenacious residual liver cancer cells, we could drastically lower the chances of recurrence,” she remarked.
Conclusion
This study illuminates the often-overlooked intricacies of tumor microenvironments and their significant relationship with cancer resilience. It underscores the importance of spatial interactions among cells and presents new avenues for therapeutic strategies against liver cancer.
Researchers from Enable Medicine and Aarhus University also contributed to this pivotal study, which received funding from the National Institutes of Health and other prominent cancer research organizations.
Could this be the breakthrough that changes the future of liver cancer treatment? Only time will tell. Keep your eyes peeled as this intriguing work continues to unfold!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)