Shocking Findings Reveal Impact of Gestational Diabetes on Newborns' Health: A Multicenter Study from Iran
2025-04-09
Author: Siti
Overview
Gestational diabetes mellitus (GDM) is becoming increasingly prevalent worldwide, with serious implications for maternal and neonatal health. This retrospective cohort study conducted across four hospitals in Iran sheds light on how GDM affects umbilical cord arterial blood gas (ABG) measurements in newborns, revealing alarming insights into the condition's impact on fetal oxygen delivery.
What You Need to Know About GDM and Pregnancy Outcomes
GDM, characterized by elevated blood glucose levels during pregnancy, can lead to a host of complications, including oversized infants (macrosomia) and low blood sugar in newborns (neonatal hypoglycemia). As the global incidence of GDM continues to rise—reportedly 21.1 million pregnancies in 2021, with GDM accounting for about 80%—healthcare providers are increasingly concerned about its adverse outcomes. A critical aspect of this study is establishing the connection between GDM and placental function, particularly how it influences fetal oxygen delivery—a topic that still lacks comprehensive evidence.
The Study: A Closer Look at the Methodology
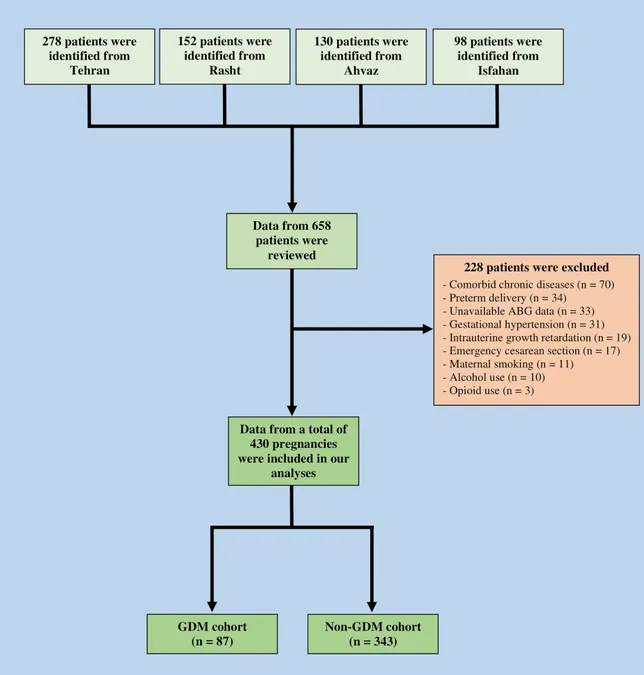
This multicenter retrospective study involved the analysis of medical records from 430 singleton-term pregnancies that underwent elective cesarean sections between January and July 2024 across Tehran, Rasht, Ahvaz, and Isfahan. The researchers excluded patients based on specific criteria including pre-existing health conditions and illegal substance use during pregnancy, aiming to isolate the effects of GDM on newborns.
Blood samples were collected from the umbilical cord immediately post-delivery to measure crucial ABG parameters: pH, partial pressure of carbon dioxide (PCO2), partial pressure of oxygen (PO2), bicarbonate levels (HCO3), and base deficit. The findings aimed not only to quantify the biological impact on infants from diabetic and non-diabetic pregnancies but also to correlate these values with secondary neonatal outcomes.
Results That Will Make You Think Twice
Among 430 pregnancies analyzed, 87 were identified as cases of GDM. The results revealed significantly lower pH levels (7.33 vs. 7.36) in the umbilical cord blood of GDM infants, alongside an increased base deficit, indicating greater metabolic acidosis. Miraculously, while no significant differences were found in other gas measurements (PCO2, PO2, HCO3), a striking 28.7% of GDM newborns required resuscitation at birth compared to only 12% of those without GDM, with NICU admissions also trending higher at 34.5% versus 16.9%.
These findings highlight the heightened risk of respiratory distress and other complications in GDM infants. Although Apgar scores—assessments of an infant's initial well-being—did not differ significantly, the clear necessity for more resuscitation and medical intervention creates a concerning picture.
The Implications of Acidic Blood in Newborns
Lower pH levels in cord blood among GDM infants suggest impaired placental function and reduced oxygenation, raising alarms not just for immediate health but for potential long-term neurodevelopmental outcomes. Chronic fetal hypoxia could lead to complications like hypoglycemia and future risks such as cerebral palsy.
The study's authors emphasize the need for rigorous monitoring of GDM pregnancies, underscoring that proactive measures, including constant glucose management and enhanced fetal surveillance, could drastically improve outcomes. Ongoing support through rapid postpartum assessments could also counteract adverse effects, ensuring a safer transition for infants affected by GDM.
What Lies Ahead: Optimizing Management Strategies
This study opens the door for critical dialogue around how healthcare practices can better support women experiencing GDM. Future research should not only deepen our understanding of these associations but also explore broader strategies that incorporate nutritional support, early interventions, and community awareness initiatives.
As studies like this illuminate the stark realities faced by expecting mothers with GDM, they also reinforce the necessity for healthcare systems to be equipped with comprehensive strategies—saving lives and ensuring healthier futures for infants around the globe.
Conclusion: The Need for Action
The implications of GDM on newborns’ health cannot be overstated. As the global prevalence of GDM rises, this study reveals just how crucial proactive monitoring and effective management strategies are. Advocates for maternal and infant health must take these findings seriously—using them as a catalyst for change in prenatal care practices worldwide.
Is your community prepared to support mothers with gestational diabetes? It’s time to act! Share this article, raise awareness, and help safeguard future generations.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)