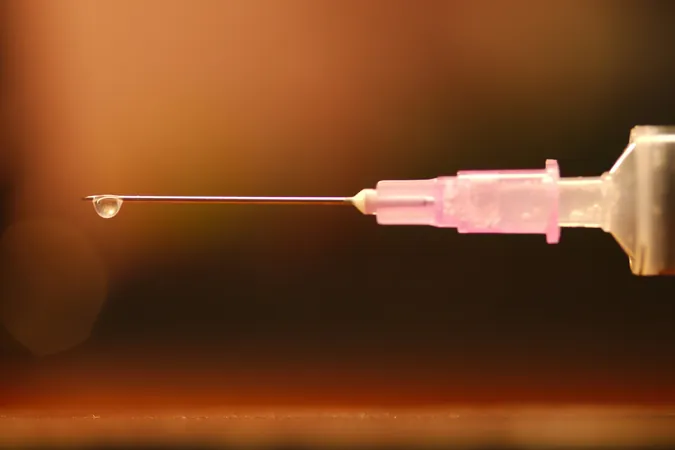
Shocking New Study Reveals Alarming Endocarditis Death Rates Among Drug Injectors – But There’s Hope!
2024-10-04
Introduction
A groundbreaking Canadian study has revealed that individuals who inject drugs are facing staggering mortality rates from endocarditis, a serious yet treatable infection affecting the heart valves. Alarmingly, the study indicates that nearly half of these patients could succumb to the condition within five years of their hospital admission. However, the research also sheds light on a glimmer of hope: comprehensive treatment, including addiction support during hospital stays, can significantly enhance survival rates.
Expert Insight
Dr. Michael Silverman, an infectious diseases researcher affiliated with St. Joseph's Health Care London and the Lawson Health Research Institute, emphasizes the gravity of endocarditis. 'This condition is not only potentially lethal but also places immense pressure on our healthcare systems. Too many lives are being lost that could otherwise be saved,' he stated, stressing the urgency of addressing this public health crisis.
Study Overview
Published in JAMA Network Open, the study conducted by Dr. Silverman in collaboration with researchers from the University of Saskatchewan, including Dr. Stuart Skinner and Dr. Cara Spence, marks the first of its kind to investigate the long-term survival rates of hospitalized patients with endocarditis between 2007 and 2023 in Ontario and Regina.
Key Findings
The statistics are staggering: among the 764 analyzed cases, approximately 56% were individuals who inject drugs (PWIDs), revealing a five-year mortality rate of 49%. With most deaths occurring within the first year, subsequent fatalities often arose from complications related to drug addiction, underscoring the pressing need for integrated care.
Gender Disparities
One of the stark revelations of this study is the disproportionate impact of endocarditis on women. Although women make up only one-third of the overall injecting drug population, they represented over 50% of the study's PWID cohort. Potential causes for this troubling trend may include social dynamics such as dependency on others for drug administration and exposure to shared injecting equipment.
Urban vs. Rural Impact
Dr. Silverman pointed out, 'We observed that women in urban areas faced higher mortality rates compared to their rural counterparts, likely due to challenges such as homelessness, violence, and the sex trade.' The absence of community support in urban settings further exacerbates the vulnerabilities faced by these women, as emphasized in the findings.
Maternal Considerations
Compounding the risks, 5% of women in the study were pregnant upon their hospital admission, highlighting an urgent need for targeted maternal care amidst a climate of high fetal and maternal mortality. Researchers assert that access to contraceptive options is a critical yet often overlooked component of care for these marginalized populations.
Call to Action
The need for immediate action is palpable. Dr. Skinner declared, 'Endocarditis among PWIDs should be deemed a health emergency. We must utilize every available resource to save lives.'
Integration of Care
Both Dr. Silverman and Dr. Spence advocate for the routine integration of addiction treatment and counseling within hospital settings, particularly for PWIDs. With their findings indicating that in-hospital support dramatically reduces premature discharges—often rooted in withdrawal symptoms—it's clear that the healthcare system must adapt to meet these patients' needs.
Conclusions
The study serves as a wake-up call for healthcare providers across North America, where many hospitals lack the comprehensive care models demonstrated to improve outcomes. As both a human rights and public health issue, it is essential that society extends empathy and enhanced healthcare access to these vulnerable populations. After all, these individuals are daughters, sons, and parents—many facing life-threatening conditions far too early in their lives.
Policy Implications
To provide effective care, policymakers must recognize the significance of community support and integrated health services. The implications of this study are far-reaching and stress the importance of transforming hospital practices to save lives and foster healthier futures for individuals grappling with addiction.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)